The glossopharyngeal nerve is a complex cranial nerve that can be associated with significant pain when affected. Understanding the various aspects of this nerve is crucial in identifying the location and intensity of pain associated with it. This article aims to provide comprehensive information about the glossopharyngeal nerve, glossopharyngeal neuralgia, pain points, diagnostic procedures, treatment options, and living with glossopharyngeal neuralgia.
Understanding the Glossopharyngeal Nerve
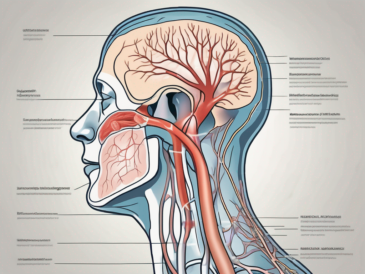
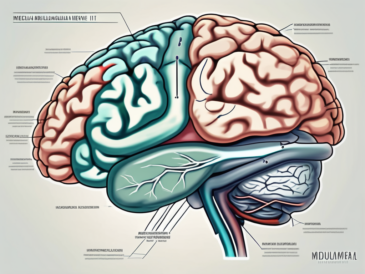
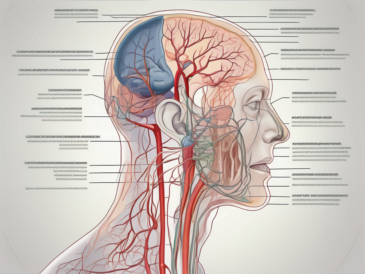
The glossopharyngeal nerve, also known as the ninth cranial nerve, is responsible for sensory and motor functions in the head and neck region. It originates in the medulla oblongata, a vital part of the brainstem, and has multiple branches that provide innervation to various structures, including the tongue, throat, and tonsils.
The glossopharyngeal nerve is a complex network of nerve fibers that serves important functions in the human body. Let’s delve deeper into the anatomy and function of this fascinating cranial nerve.
Anatomy of the Glossopharyngeal Nerve
The glossopharyngeal nerve consists of sensory and motor fibers. The sensory fibers carry information related to taste, touch, and pain from the posterior third of the tongue, the soft palate, and the tonsils. These sensory signals are crucial for our ability to perceive and enjoy the flavors of the food we eat.
Additionally, the glossopharyngeal nerve plays a role in the gag reflex, which helps protect the airway by triggering a reflexive contraction of the throat muscles when an object touches the back of the throat.
The motor fibers of the glossopharyngeal nerve control the muscles involved in swallowing and speech. These muscles work in harmony to ensure the smooth passage of food and liquids from the mouth to the esophagus, allowing us to eat and drink without difficulty.
Function of the Glossopharyngeal Nerve
The glossopharyngeal nerve plays a crucial role in various functions, including taste perception, swallowing, saliva production, and regulation of blood pressure. Taste perception is a complex process that involves the activation of taste buds on the tongue, and the glossopharyngeal nerve carries the sensory signals from these taste buds to the brain, allowing us to savor the flavors of different foods.
In addition to taste perception, the glossopharyngeal nerve is involved in the production of saliva. Saliva is essential for lubricating the mouth, aiding in digestion, and maintaining oral health. The glossopharyngeal nerve stimulates the salivary glands to produce saliva, ensuring that our mouths stay moist and comfortable.
Furthermore, the glossopharyngeal nerve plays a role in regulating blood pressure. It relays sensory information from the carotid sinus, a specialized area in the carotid artery that helps monitor blood pressure and oxygen levels. This information is crucial for maintaining cardiovascular homeostasis and ensuring that our bodies receive adequate oxygen and nutrients.
The glossopharyngeal nerve is a remarkable cranial nerve that contributes to various essential functions in the head and neck region. Its intricate anatomy and multifaceted functions make it a fascinating subject of study in the field of neuroscience. Understanding the glossopharyngeal nerve helps us appreciate the complexity of the human body and the interconnectedness of its various systems.
Identifying Glossopharyngeal Neuralgia
Glossopharyngeal neuralgia is a condition characterized by recurrent, severe pain in the distribution of the glossopharyngeal nerve. It is considered rare but can cause significant discomfort and impact the quality of life for those affected.
The glossopharyngeal nerve, also known as the ninth cranial nerve, is responsible for providing sensory and motor innervation to the throat, tongue, and ear. When this nerve becomes irritated or compressed, it can result in the development of glossopharyngeal neuralgia.
Individuals with glossopharyngeal neuralgia often experience intense, stabbing pain in the throat, tongue, and/or ear. These pain episodes can be triggered by various activities, such as swallowing, talking, or even touching specific areas, such as the tonsils. The pain is often described as sharp, shooting, or electric-like in nature.
In addition to the primary symptom of pain, individuals with glossopharyngeal neuralgia may also experience difficulty swallowing, voice changes, and occasional syncope (fainting). These additional symptoms can further impact daily activities and overall well-being.
Symptoms of Glossopharyngeal Neuralgia
The primary symptom of glossopharyngeal neuralgia is intense, stabbing pain in the throat, tongue, and/or ear. The pain episodes can be triggered by activities such as swallowing, talking, or even touching specific areas, such as the tonsils. Other symptoms may include difficulty swallowing, voice changes, and occasional syncope (fainting).
Difficulty swallowing, also known as dysphagia, can occur due to the pain and discomfort associated with glossopharyngeal neuralgia. This can lead to challenges in consuming food and liquids, potentially resulting in weight loss and malnutrition if not properly managed.
Voice changes can also be a significant symptom of glossopharyngeal neuralgia. The pain and irritation in the throat can affect the vocal cords, leading to hoarseness, changes in pitch, and a strained voice. This can impact communication and may require speech therapy to help improve vocal function.
Occasional syncope, or fainting, can occur as a result of the intense pain experienced during glossopharyngeal neuralgia episodes. The body’s response to severe pain can cause a sudden drop in blood pressure, leading to loss of consciousness. It is important for individuals with glossopharyngeal neuralgia to be aware of this potential symptom and take precautions to prevent injury during episodes.
Causes of Glossopharyngeal Neuralgia
Glossopharyngeal neuralgia can be caused by various factors, including compression of the nerve by nearby vessels or tumors, irritation from infections or trauma, or even idiopathic (unknown) causes. It is vital to consult with a healthcare professional to determine the underlying cause and develop an appropriate management plan.
Compression of the glossopharyngeal nerve by nearby blood vessels, such as the arteries that supply blood to the brain, can lead to glossopharyngeal neuralgia. The pressure exerted on the nerve can result in irritation and the development of pain symptoms. In some cases, surgical intervention may be necessary to relieve the compression and alleviate the pain.
Tumors, both benign and malignant, can also contribute to the development of glossopharyngeal neuralgia. When a tumor grows in close proximity to the glossopharyngeal nerve, it can compress or irritate the nerve, leading to the onset of symptoms. Treatment of the tumor may involve surgery, radiation therapy, or a combination of both.
Infections, such as viral or bacterial infections, can cause inflammation and irritation of the glossopharyngeal nerve, resulting in glossopharyngeal neuralgia. Trauma to the throat or head region can also lead to nerve damage and subsequent pain. Identifying and treating the underlying infection or addressing the trauma is crucial in managing glossopharyngeal neuralgia.
While the exact cause of glossopharyngeal neuralgia is not always known, it is important to explore potential underlying factors to guide treatment and management. A thorough evaluation by a healthcare professional, including a detailed medical history, physical examination, and possibly imaging studies, can help determine the cause and develop an appropriate plan of care.
Pain Location and Intensity
The location and intensity of pain associated with glossopharyngeal neuralgia can vary from person to person. It is crucial to identify the specific pain points and understand the factors that influence pain intensity.
Glossopharyngeal neuralgia is a rare condition characterized by severe, stabbing pain in the throat, tongue, ear, and jaw. The pain is often described as sharp and electric shock-like, causing significant discomfort and distress to those affected. While the exact cause of glossopharyngeal neuralgia is not fully understood, it is believed to be related to irritation or compression of the glossopharyngeal nerve, which is responsible for transmitting sensory information from the throat and tongue to the brain.
When it comes to pain location, glossopharyngeal neuralgia typically originates at the back of the tongue or throat and can radiate to the ear or jaw. The pain may be unilateral, affecting only one side, or bilateral, affecting both sides. The episodes of pain can vary in duration, ranging from a few seconds to several minutes. This variability in pain presentation underscores the importance of a comprehensive evaluation by healthcare professionals to accurately diagnose glossopharyngeal neuralgia.
Pain Points Associated with Glossopharyngeal Neuralgia
The specific trigger points and pain distribution in glossopharyngeal neuralgia can vary among individuals. Some may experience pain primarily in the throat, while others may feel it more intensely in the tongue or jaw. The pain can also extend to the ear, causing a deep, throbbing sensation that worsens with movement or swallowing. These diverse pain points highlight the complex nature of glossopharyngeal neuralgia and the need for personalized treatment approaches.
During episodes of glossopharyngeal neuralgia, individuals may find it challenging to speak, eat, or even perform simple daily activities due to the excruciating pain. The pain can be triggered by various factors, such as talking, chewing, swallowing, or even touching specific areas in the mouth. Understanding these trigger points is crucial in managing and preventing pain episodes, as it allows individuals to modify their behaviors and avoid activities that exacerbate their symptoms.
Factors Influencing Pain Intensity
The intensity of glossopharyngeal neuralgia pain can be influenced by various factors. Stress levels play a significant role in triggering or worsening pain episodes. High levels of stress can lead to muscle tension and increased sensitivity, making individuals more susceptible to pain. Similarly, physical exertion or strenuous activities can aggravate glossopharyngeal neuralgia symptoms, causing a spike in pain intensity.
Temperature changes can also impact the severity of glossopharyngeal neuralgia pain. Exposure to extreme hot or cold temperatures, such as drinking hot or cold beverages, can trigger or intensify pain episodes. Understanding these environmental factors and making necessary adjustments, such as avoiding extreme temperatures, can help individuals better cope with the pain associated with glossopharyngeal neuralgia.
In conclusion, glossopharyngeal neuralgia is a complex condition characterized by varying pain locations and intensities. The pain can originate in the throat, tongue, ear, or jaw and may be triggered by factors such as stress, physical exertion, and temperature changes. By identifying these pain points and understanding the factors that influence pain intensity, individuals can work with healthcare professionals to develop personalized strategies for managing and alleviating glossopharyngeal neuralgia symptoms.
Diagnostic Procedures for Glossopharyngeal Neuralgia
Diagnosing glossopharyngeal neuralgia typically involves a thorough medical history assessment, physical examination, and specific imaging tests to identify the underlying cause.
Glossopharyngeal neuralgia is a rare condition characterized by severe, recurring pain in the throat, tongue, and ear. The pain is often described as sharp, stabbing, or electric shock-like. It can be triggered by simple activities such as swallowing, talking, or even touching the face. To accurately diagnose glossopharyngeal neuralgia, healthcare professionals employ a variety of diagnostic procedures.
Medical History and Physical Examination
A detailed medical history and physical examination are crucial in determining the presence and characteristics of glossopharyngeal neuralgia. The healthcare professional will inquire about the nature of pain, triggers, and associated symptoms. They will ask about the frequency and duration of the pain episodes, as well as any factors that seem to alleviate or worsen the symptoms. Additionally, they will assess the patient’s medical history, looking for any underlying conditions or previous injuries that may contribute to the development of glossopharyngeal neuralgia.
During the physical examination, the healthcare professional will perform various tests to evaluate the patient’s cranial nerve functions. They will assess the sensation and motor function of the face, throat, and tongue. By carefully examining these areas, they can identify any abnormalities or signs of nerve damage that may be indicative of glossopharyngeal neuralgia.
Imaging Tests and Their Role
Imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT), may be required to visualize the glossopharyngeal nerve and surrounding structures. These tests help identify potential compressions, tumors, or structural abnormalities that may contribute to glossopharyngeal neuralgia.
An MRI uses powerful magnets and radio waves to create detailed images of the body’s internal structures. It can provide a clear view of the glossopharyngeal nerve and detect any abnormalities, such as nerve compression caused by blood vessels or tumors.
On the other hand, a CT scan uses X-rays and computer technology to produce cross-sectional images of the body. It can reveal any structural abnormalities, such as bone spurs or cysts, that may be affecting the glossopharyngeal nerve.
These imaging tests are non-invasive and painless. They allow healthcare professionals to get a better understanding of the underlying cause of glossopharyngeal neuralgia and determine the most appropriate treatment approach.
Treatment Options for Glossopharyngeal Neuralgia
The management of glossopharyngeal neuralgia focuses on pain relief and improving quality of life. Treatment options may involve medication and various surgical interventions.
Glossopharyngeal neuralgia is a rare condition characterized by severe, recurring pain in the throat, tongue, and ear. The pain can be triggered by simple activities such as talking, swallowing, or even just touching the face. This debilitating condition can significantly impact a person’s daily life, making it crucial to explore effective treatment options.
Medication for Pain Management
Medications, such as anticonvulsants and tricyclic antidepressants, may be prescribed to reduce neuralgia pain. These medications aim to stabilize nerve activity and provide relief. Anticonvulsants, such as carbamazepine or gabapentin, work by inhibiting abnormal electrical activity in the nerves, while tricyclic antidepressants, like amitriptyline, can help modulate pain signals in the brain.
It is essential to work closely with a healthcare professional to find the most suitable medication and dosage. They will consider factors such as the severity of the pain, the patient’s overall health, and any potential side effects. Regular follow-ups and adjustments to the medication may be necessary to ensure optimal pain management.
Surgical Interventions and Their Effectiveness
In cases where conservative measures fail to alleviate pain, surgical interventions may be considered. These can include microvascular decompression, radiofrequency ablation, or nerve blocks.
Microvascular decompression is a surgical procedure that involves placing a cushioning material between the glossopharyngeal nerve and the blood vessels compressing it. This helps to relieve pressure on the nerve and reduce pain. Radiofrequency ablation, on the other hand, uses heat generated by radio waves to destroy the problematic nerve fibers, effectively blocking pain signals.
Nerve blocks, such as glossopharyngeal nerve blocks, involve injecting a local anesthetic into the affected nerve to temporarily numb it and provide relief. These blocks can be performed as a diagnostic tool to determine the source of the pain or as a therapeutic measure to alleviate symptoms.
However, the decision to pursue surgical options should be undertaken in consultation with a healthcare professional specializing in the management of cranial nerve disorders. They will evaluate the patient’s specific case and consider factors such as the severity of the pain, the patient’s overall health, and the potential risks and benefits of each surgical intervention.
It is important to note that while surgical interventions can provide significant pain relief for some individuals, they may not be suitable or effective for everyone. Each person’s experience with glossopharyngeal neuralgia is unique, and treatment plans should be tailored to their specific needs and circumstances.
Living with Glossopharyngeal Neuralgia
Living with glossopharyngeal neuralgia can be challenging, given the unpredictable nature of pain episodes. However, there are lifestyle adjustments and strategies that can help individuals cope with chronic pain and improve their overall well-being.
Lifestyle Adjustments for Pain Management
Engaging in stress-reducing activities, such as meditation or yoga, following a healthy diet, and getting regular exercise can help manage glossopharyngeal neuralgia symptoms. It is advisable to avoid triggers, such as excessively cold or hot foods, and maintain good oral hygiene to minimize potential irritations.
Psychological Impact of Chronic Pain
Chronic pain can have a significant psychological impact on individuals. It is important to seek support from healthcare professionals, counselors, or support groups to address any anxiety, depression, or emotional challenges that may arise from living with glossopharyngeal neuralgia.
In conclusion, pain associated with the glossopharyngeal nerve can occur in various locations and intensities. Glossopharyngeal neuralgia is a complex condition that requires a thorough evaluation for accurate diagnosis and appropriate management. It is crucial to consult with a healthcare professional who specializes in cranial nerve disorders to develop an individualized treatment plan. With proper care and management strategies, individuals living with glossopharyngeal neuralgia can lead fulfilling lives while effectively managing chronic pain.