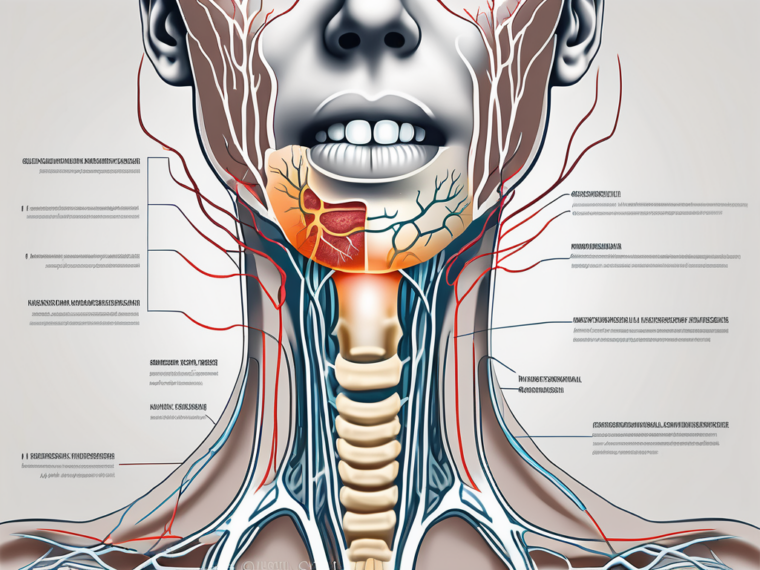
The throat is a complex and vital part of the human anatomy, responsible for various functions such as swallowing, speaking, and breathing. Two key nerves, the vagus nerve and the glossopharyngeal nerve, play a crucial role in innervating the throat and facilitating these essential functions. In this article, we will delve into the intricacies of these nerves, exploring their anatomy, function, interplay, associated disorders, and the future of neurological research in throat innervation.
Understanding the Vagus Nerve
Anatomy and Function of the Vagus Nerve
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It extends from the brainstem and branches out into various regions of the body, including the throat. The vagus nerve plays a crucial role in regulating several vital functions, such as heart rate, digestion, and respiration. In addition to these essential functions, the vagus nerve also has a profound impact on the throat and its intricate mechanisms.
The throat, a vital part of the upper respiratory and digestive systems, relies heavily on the vagus nerve for its proper functioning. This nerve is responsible for controlling the muscles involved in swallowing and speech, ensuring the smooth passage of food and liquids from the mouth into the esophagus and beyond. Without the vagus nerve’s motor signals, the intricate coordination required for swallowing would be disrupted, leading to difficulties in eating and drinking.
Role of the Vagus Nerve in Throat Innervation
When it comes to innervating the throat, the vagus nerve plays a central role. It sends motor signals to the muscles responsible for swallowing, allowing food and liquids to pass from the mouth into the esophagus and beyond. These muscles, including the pharyngeal constrictors and the muscles of the larynx, work in harmony under the guidance of the vagus nerve to ensure the efficient movement of ingested substances through the throat.
Moreover, the vagus nerve carries sensory information from the throat, providing feedback on pain, temperature, and pressure. This sensory feedback is crucial for detecting and responding to potential threats or abnormalities in the throat. It allows us to sense discomfort, such as the presence of a foreign object or the sensation of burning, and take appropriate actions to protect our airways and maintain our overall well-being.
The intricate interplay between motor and sensory functions of the vagus nerve ensures the efficient functioning of the throat. It is responsible for the coordination of the muscles involved in swallowing, preventing the entry of food or liquids into the airway, and facilitating the passage of ingested substances into the digestive system. Additionally, the vagus nerve’s sensory feedback helps us detect and respond to potential dangers or abnormalities, ensuring the protection and health of our throat.
Delving into the Glossopharyngeal Nerve
Structure and Purpose of the Glossopharyngeal Nerve
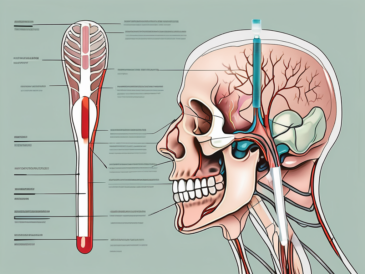
The glossopharyngeal nerve, the ninth cranial nerve, follows a similar path to the vagus nerve, originating from the brainstem. Just like the vagus nerve, the glossopharyngeal nerve has both motor and sensory functions. In the throat, the glossopharyngeal nerve innervates the muscles involved in swallowing and speech, similar to the vagus nerve but with a slightly different distribution.
The glossopharyngeal nerve is a complex network of nerve fibers that plays a crucial role in the functioning of the throat. It is responsible for transmitting signals between the brain and the muscles involved in swallowing and speech. Without the glossopharyngeal nerve, these essential functions would be impaired, leading to difficulties in eating, drinking, and communicating.
Furthermore, the glossopharyngeal nerve is not only involved in motor functions but also carries sensory information from the throat and tongue. This sensory input allows us to perceive taste and respond accordingly, adding to the overall sensory experience of eating and drinking. The taste signals transmitted by the glossopharyngeal nerve contribute to our ability to savor and enjoy different flavors, enhancing the pleasure of consuming food and beverages.
The Glossopharyngeal Nerve’s Part in Throat Innervation
The glossopharyngeal nerve enables the coordinated movement of the muscles in the throat, ensuring the proper passage of food and liquids during swallowing. It works in conjunction with other cranial nerves to orchestrate the complex sequence of muscle contractions required for efficient swallowing. This intricate coordination ensures that the food we consume is safely transported from the mouth to the esophagus, preventing choking and facilitating digestion.
In addition to its role in swallowing, the glossopharyngeal nerve also plays a vital part in speech production. It innervates the muscles involved in articulation, allowing us to produce a wide range of sounds and communicate effectively. Without the glossopharyngeal nerve’s contribution to throat innervation, our ability to speak clearly and express ourselves verbally would be severely compromised.
Moreover, the glossopharyngeal nerve’s involvement in throat innervation extends beyond motor functions. It carries sensory information from the back of the throat and the tongue, allowing us to perceive various tastes. This sensory input is crucial for our enjoyment of food and beverages, as it enables us to distinguish between different flavors and appreciate the nuances of taste. The glossopharyngeal nerve’s role in throat innervation, therefore, not only ensures the proper functioning of essential bodily processes but also enhances our sensory experiences.
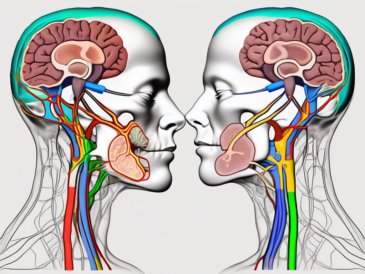
The Interplay Between the Vagus and Glossopharyngeal Nerves
How These Two Nerves Work Together
The vagus nerve and the glossopharyngeal nerve work in tandem to facilitate the complex movements and sensations in the throat. Their combined efforts ensure efficient swallowing, speaking, and sensory perception. The motor signals from both nerves coordinate the contraction of various throat muscles in a synchronized manner, while the sensory signals provide important feedback to the brain for perception and response.
Let’s delve deeper into the intricate coordination between these two nerves. The vagus nerve, also known as cranial nerve X, is the longest cranial nerve in the body. It originates in the brainstem and branches out extensively, innervating various organs and structures, including the throat. This nerve plays a crucial role in regulating the parasympathetic nervous system, which is responsible for controlling involuntary bodily functions.
The glossopharyngeal nerve, on the other hand, is cranial nerve IX. It also originates in the brainstem and carries both motor and sensory fibers. This nerve innervates the tongue, throat, and part of the ear, contributing to taste perception, swallowing, and speech.
When these two nerves work together, they ensure the smooth functioning of the throat. The motor signals from the vagus nerve stimulate the contraction of muscles involved in swallowing, such as the pharyngeal constrictors and the esophagus, in a coordinated manner. Simultaneously, the glossopharyngeal nerve provides sensory feedback, allowing the brain to monitor the process and make necessary adjustments if needed.
Impact on Throat Function and Sensation
When either the vagus or glossopharyngeal nerve experiences dysfunction, it can have a significant impact on throat function and sensation. Difficulties in swallowing, known as dysphagia, can arise, leading to potential aspiration or malnutrition. Speech may also be affected, resulting in changes in vocal quality or difficulty articulating words.
Disrupted sensory feedback from these nerves can reduce taste perception and impair the overall sensory experience associated with eating and drinking. Taste buds on the tongue rely on the glossopharyngeal nerve to transmit taste signals to the brain, allowing us to savor the flavors of different foods and beverages. Without proper functioning of this nerve, the ability to fully enjoy and appreciate the taste of food may be compromised.
Furthermore, the vagus nerve plays a crucial role in regulating the gag reflex, which is a protective mechanism to prevent choking. Dysfunction in this nerve can lead to an exaggerated or diminished gag reflex, potentially increasing the risk of choking or aspiration.
It is important to note that various factors can contribute to the dysfunction of these nerves. Injuries, infections, tumors, and certain medical conditions can all affect the proper functioning of the vagus and glossopharyngeal nerves. Prompt diagnosis and appropriate treatment are essential to restore normal throat function and sensation.
Disorders Related to Vagus and Glossopharyngeal Nerve Dysfunction
Symptoms and Diagnosis
Disorders related to dysfunction of the vagus and glossopharyngeal nerves can manifest in various ways. Common symptoms include difficulty swallowing, hoarseness, changes in taste perception, and throat pain. These symptoms can significantly impact a person’s quality of life, making it essential to seek medical attention for a proper diagnosis.
When a person experiences difficulty swallowing, it can lead to a range of complications, including malnutrition and dehydration. This is because the act of swallowing is a complex process that involves the coordination of multiple muscles and nerves. Dysfunction of the vagus and glossopharyngeal nerves can disrupt this coordination, leading to a feeling of food getting stuck in the throat or even choking episodes.
Hoarseness, another common symptom of vagus and glossopharyngeal nerve dysfunction, can be caused by the disruption of the vocal cord muscles. These muscles, controlled by the vagus nerve, are responsible for producing sound during speech. When the nerve function is compromised, the vocal cords may not be able to vibrate properly, resulting in a hoarse or weak voice.
Changes in taste perception can also occur when there is dysfunction of the glossopharyngeal nerve. This nerve is responsible for transmitting taste signals from the back of the tongue to the brain. When the nerve is not functioning correctly, it can lead to a distorted sense of taste or a loss of taste altogether.
Throat pain is a common complaint among individuals with vagus and glossopharyngeal nerve dysfunction. This pain can range from a mild discomfort to a sharp, stabbing sensation. It can be localized or radiate to other areas of the head and neck. The exact cause of the throat pain can vary, ranging from inflammation of the nerves to muscle spasms.
When a person presents with these symptoms, doctors may perform clinical examinations, imaging studies, or electrophysiological tests to pinpoint the underlying cause of the nerve dysfunction. Clinical examinations may involve assessing the strength and coordination of the muscles involved in swallowing and speech. Imaging studies, such as MRI or CT scans, can provide detailed images of the nerves and surrounding structures. Electrophysiological tests, such as nerve conduction studies, can measure the electrical activity of the nerves to assess their function.
Treatment and Management Options
The treatment and management of vagus and glossopharyngeal nerve disorders depend on the underlying cause and severity of the condition. In some cases, medication or dietary modifications may be sufficient to alleviate the symptoms. For example, medications that reduce inflammation or relax muscles can help relieve throat pain and improve swallowing function.
Dietary modifications may involve adjusting the texture or consistency of food to make swallowing easier. Thickening agents can be added to liquids to prevent choking, and pureed or soft foods may be recommended to reduce the risk of aspiration.
However, more severe cases of vagus and glossopharyngeal nerve dysfunction may require surgical interventions or rehabilitative therapies to restore throat function and sensation. Surgical options can include nerve decompression, where the affected nerves are released from any compression or entrapment, or nerve grafting, where a healthy nerve is used to repair or replace the damaged one.
Rehabilitative therapies, such as speech therapy and swallowing exercises, can help improve muscle strength and coordination, allowing individuals to regain their ability to swallow and speak effectively.
It is vital to consult with a healthcare professional to determine the most appropriate treatment plan for individual circumstances. They can assess the underlying cause of the nerve dysfunction and tailor a treatment approach that addresses the specific needs of the patient. With proper diagnosis and management, individuals with vagus and glossopharyngeal nerve dysfunction can experience improved quality of life and regain their ability to eat, speak, and enjoy food without discomfort or limitations.
The Future of Neurological Research in Throat Innervation
Neurological research in throat innervation is an area of ongoing exploration that holds promise for future advancements in diagnosis and treatment. The intricate workings of the throat are governed by a complex network of nerves, including the vagus and glossopharyngeal nerves. These nerves play vital roles in innervating the throat and facilitating its functions.
Techniques such as neuroimaging and electrophysiology are providing greater insights into the function and connectivity of the vagus and glossopharyngeal nerves. Neuroimaging techniques, such as functional magnetic resonance imaging (fMRI), allow researchers to visualize brain activity associated with throat innervation. This enables a better understanding of how the brain processes sensory information and controls motor functions in the throat. Electrophysiology, on the other hand, involves the measurement of electrical activity in the nerves, providing valuable information about their function and potential abnormalities.
Advancements in neuromodulation and bioengineering also hold potential in the field of throat innervation research. Neuromodulation techniques, such as vagus nerve stimulation, involve the use of electrical impulses to modulate nerve activity. This approach has shown promise in treating various neurological conditions and may offer a means to restore compromised throat function by stimulating or bypassing damaged nerves. Bioengineering approaches, on the other hand, aim to develop artificial devices or materials that can mimic the function of damaged nerves, providing a potential avenue for restoring throat function.
Potential Implications for Patient Care
As research in throat innervation advances, the potential implications for patient care are significant. Improved diagnostics can lead to earlier detection and intervention in cases of nerve dysfunction, enhancing patient outcomes and quality of life. Early detection of nerve abnormalities can allow for targeted interventions, such as physical therapy or surgical interventions, to prevent further deterioration and promote recovery.
Additionally, novel therapeutic approaches may offer alternative treatment options for individuals who do not respond to traditional methods. For example, individuals with swallowing difficulties due to nerve damage may benefit from neuromodulation techniques that can help stimulate the muscles involved in swallowing. These advancements have the potential to significantly improve the quality of life for patients with throat innervation disorders.
However, it is essential to note that these advancements are still in the early stages and should be approached with caution. While the potential benefits are promising, further research is needed to fully understand the long-term effectiveness and safety of these techniques. It is crucial to seek professional medical advice and guidance when considering any new treatment options.
In conclusion, the vagus nerve and the glossopharyngeal nerve play vital roles in innervating the throat and facilitating its functions. From motor control during swallowing and speech to sensory perception of taste and feedback, these nerves contribute to the intricate workings of the throat. Understanding their anatomy, function, and interplay is crucial in diagnosing and managing disorders related to their dysfunction.
Ongoing neurological research holds great potential for advancements in throat innervation, offering hope for improved diagnostics and treatments in the future. If you experience any difficulties or symptoms related to throat function, it is important to consult with a healthcare professional for a comprehensive evaluation and appropriate management. The future of neurological research in throat innervation is bright, and with continued advancements, we may unlock new possibilities for enhancing the well-being of individuals with throat innervation disorders.