The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a crucial role in various functions within the body. From controlling the muscles involved in swallowing and speaking to providing sensory input from the tongue, throat, and certain internal organs, this nerve is essential for normal functioning. However, when it becomes damaged, it can lead to a range of symptoms and challenges that affect an individual’s quality of life. In this article, we will explore the various aspects related to glossopharyngeal nerve damage, including its anatomy, causes, symptoms, diagnosis, treatment options, prognosis, and prevention measures.
Understanding the Glossopharyngeal Nerve
The glossopharyngeal nerve is a complex cranial nerve that plays a crucial role in various functions of the head and neck. Let’s delve deeper into the anatomy and functions of this fascinating nerve.
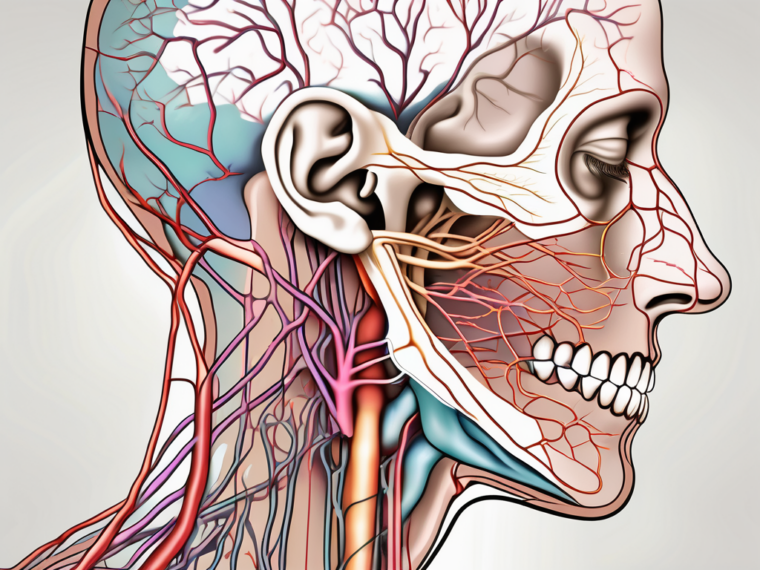
Anatomy of the Glossopharyngeal Nerve
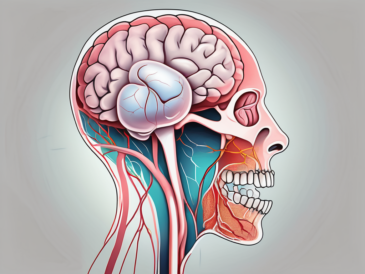
The glossopharyngeal nerve arises from the brainstem, specifically the medulla oblongata. This region, located at the base of the brain near the spinal cord, serves as the origin for many important nerves. The glossopharyngeal nerve emerges from the medulla oblongata and travels through the skull, passing through various structures along its path.
As it branches out, the glossopharyngeal nerve innervates several structures, including the tongue, tonsils, pharynx, and various glands. Its extensive reach allows it to control essential functions related to swallowing, taste perception, and blood pressure regulation.
One intriguing aspect of the glossopharyngeal nerve is its connection to the carotid sinus. This specialized structure, located in the carotid artery, plays a vital role in monitoring and regulating blood pressure. The glossopharyngeal nerve carries sensory information from the carotid sinus to the brain, allowing for precise control and adjustment of blood pressure levels.
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve exhibits a wide range of functions, encompassing both motor and sensory capabilities. Understanding these functions provides insight into the nerve’s importance in maintaining various physiological processes.
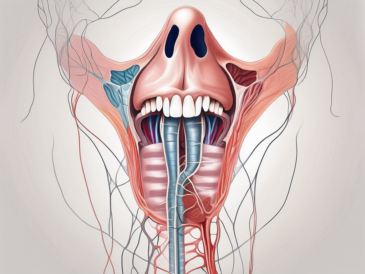
On the motor side, the glossopharyngeal nerve controls the movement of specific muscles involved in swallowing. The muscles of the pharynx and soft palate rely on the signals transmitted by this nerve to coordinate the complex actions required for efficient swallowing. Additionally, the glossopharyngeal nerve stimulates the salivary glands, contributing to the production of saliva, which aids in digestion and oral health.
Turning our attention to the sensory functions, the glossopharyngeal nerve is responsible for relaying information related to taste, touch, and pain sensations. Specifically, it carries signals from the posterior third of the tongue, upper throat, and areas near the tonsils. This sensory input allows us to perceive and differentiate tastes, ensuring an enjoyable and diverse culinary experience.
Moreover, the glossopharyngeal nerve plays a crucial role in monitoring blood pressure through its connection to the carotid sinus. By transmitting signals from this specialized structure to the brain, the nerve enables the body to maintain optimal blood pressure levels, contributing to overall cardiovascular health.
Understanding the intricate anatomy and functions of the glossopharyngeal nerve highlights its significance in our daily lives. From facilitating the act of swallowing to allowing us to savor the flavors of our favorite foods, this nerve plays a vital role in maintaining our well-being.
Causes of Glossopharyngeal Nerve Damage
The glossopharyngeal nerve is a crucial component of the human nervous system, responsible for carrying sensory and motor signals between the brain and the throat, tongue, and other vital structures in the head and neck region. While it plays a vital role in our daily lives, there are several factors that can lead to glossopharyngeal nerve damage. Understanding these causes can help individuals take preventative measures and seek appropriate treatment when necessary.
Trauma and Injury
Glossopharyngeal nerve damage can occur as a result of various traumatic events. For instance, a severe head injury, such as a concussion or skull fracture, may impact the nerve’s integrity. The forceful impact on the head can disrupt the delicate nerve fibers, leading to a range of symptoms and complications. Additionally, physical trauma caused by accidents, falls, or surgical procedures involving the head and neck region can also lead to nerve damage. It is important to understand that any injury to the area surrounding the glossopharyngeal nerve can potentially affect its functioning.
Individuals involved in high-risk activities or occupations should take extra precautions to protect their head and neck from potential injuries. Wearing appropriate safety gear, such as helmets or protective headgear, can significantly reduce the risk of trauma to the glossopharyngeal nerve and other vital structures in the region.
Surgical Complications
While surgical interventions are sometimes necessary to address certain medical conditions, complications can arise that may inadvertently affect the glossopharyngeal nerve. Procedures involving the removal of tonsils, tumors, or other structures in close proximity to the nerve carry a risk of damage. Surgeons carefully assess each case to minimize such risks, taking into consideration the nerve’s location and vulnerability. However, unfortunately, unforeseen circumstances can arise, leading to potential nerve injury.
Patients undergoing surgical procedures in the head and neck region should have a thorough discussion with their healthcare provider about the potential risks and benefits. Understanding the specific details of the procedure and the surgeon’s experience can help individuals make informed decisions and take appropriate precautions to minimize the risk of glossopharyngeal nerve damage.
Neurological Disorders
Neurological disorders can also contribute to glossopharyngeal nerve damage. Conditions such as multiple sclerosis, stroke, and tumors that affect the brainstem or nearby structures can interfere with the proper functioning of the nerve. These disorders may result in inflammation, compression, or disruption of the nerve fibers, leading to various symptoms and complications.
Individuals diagnosed with neurological disorders should work closely with their healthcare team to manage their condition effectively. Regular monitoring, appropriate medication, and lifestyle modifications can help minimize the risk of glossopharyngeal nerve damage and improve overall quality of life.
In conclusion, glossopharyngeal nerve damage can occur due to various causes, including trauma and injury, surgical complications, and neurological disorders. Understanding these causes and taking appropriate preventive measures can help individuals protect the integrity of their glossopharyngeal nerve and maintain optimal health and well-being.
Symptoms of Glossopharyngeal Nerve Damage
Physical Symptoms
Affected individuals may experience physical symptoms resulting from glossopharyngeal nerve damage. These can include difficulty swallowing, termed dysphagia, and changes in the voice, such as hoarseness or difficulty articulating certain sounds. Additionally, muscle weakness or paralysis of the muscles involved in swallowing may cause choking or coughing during meals. Some individuals may also notice a decrease in saliva production, which can result in dry mouth and difficulties with oral hygiene.
Glossopharyngeal nerve damage can have a significant impact on an individual’s ability to eat and drink. Dysphagia, or difficulty swallowing, can make it challenging to consume food and liquids safely and efficiently. This can lead to a decreased intake of nutrients and hydration, potentially resulting in weight loss, malnutrition, and dehydration. Furthermore, the changes in voice, such as hoarseness or difficulty articulating certain sounds, can affect an individual’s ability to communicate effectively, impacting social interactions and overall quality of life.
In addition to the physical symptoms mentioned above, glossopharyngeal nerve damage can also affect an individual’s ability to breathe properly. The muscles involved in swallowing also play a crucial role in protecting the airway during swallowing. When these muscles are weakened or paralyzed, there is an increased risk of aspiration, where food or liquid enters the airway instead of the esophagus. Aspiration can lead to respiratory issues, such as coughing, choking, or even pneumonia, further complicating the individual’s health and well-being.
Sensory Changes
Glossopharyngeal nerve damage can also lead to sensory changes in the affected areas. People may experience altered or decreased taste sensations, particularly at the back of the tongue. This can impact an individual’s enjoyment of food and may lead to a decreased appetite. Additionally, the feeling of numbness or tingling in the throat, tongue, or other regions served by the nerve can be unsettling and uncomfortable.
In severe cases of glossopharyngeal nerve damage, individuals may even experience intense pain in the affected areas, known as glossopharyngeal neuralgia. This condition can cause sharp, shooting, or burning pain in the throat, tongue, ear, or jaw. The pain can be triggered by various activities, such as swallowing, talking, or even touching the affected areas. Glossopharyngeal neuralgia can significantly impact an individual’s quality of life, causing distress and interfering with daily activities.
Speech and Swallowing Difficulties
Speech and swallowing difficulties can significantly impact an individual’s daily life. When the glossopharyngeal nerve is damaged, the coordination required for proper speech production and swallowing can be disrupted. This may manifest as slurred speech, difficulties forming words, or the sensation of food getting stuck in the throat. These challenges can impact communication, social interactions, and overall well-being.
Individuals with glossopharyngeal nerve damage may find it challenging to express themselves verbally, leading to frustration and potential misunderstandings. The difficulties in forming words and the sensation of food getting stuck in the throat can also cause embarrassment and self-consciousness, affecting an individual’s confidence and self-esteem. Furthermore, the impact on swallowing can lead to a fear of eating and drinking, further exacerbating the potential nutritional and hydration issues mentioned earlier.
It is important for individuals experiencing symptoms of glossopharyngeal nerve damage to seek medical attention for proper diagnosis and management. Treatment options may include medication, physical therapy, and in some cases, surgical intervention. Rehabilitation programs focusing on speech and swallowing exercises can also be beneficial in improving function and quality of life for those affected by glossopharyngeal nerve damage.
Diagnosis of Glossopharyngeal Nerve Damage
Medical History and Physical Examination
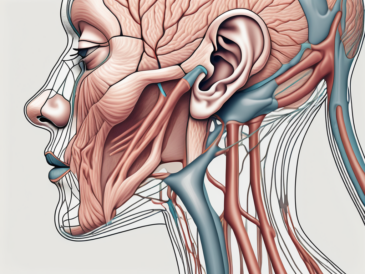
Diagnosing glossopharyngeal nerve damage begins with a thorough assessment of an individual’s medical history and symptoms. Healthcare professionals will inquire about any head injuries, surgeries, or underlying medical conditions that could contribute to nerve damage. They will also perform a physical examination, specifically focusing on the areas innervated by the glossopharyngeal nerve. This may involve assessing muscle strength, reflexes, and sensory responses.
During the medical history evaluation, the healthcare provider will ask detailed questions to gather information about the onset, duration, and progression of symptoms. They will also inquire about any associated symptoms, such as difficulty swallowing, changes in taste, or pain in the throat or ear. Understanding the timeline and characteristics of the symptoms can provide valuable clues in the diagnostic process.
The physical examination will involve a comprehensive evaluation of the head and neck region. The healthcare provider will assess the function of the glossopharyngeal nerve by examining the movement and sensation of the tongue, throat, and pharynx. They may use a tongue depressor to observe the movement of the tongue and check for any signs of weakness or asymmetry. The provider may also gently touch different areas of the throat and mouth to assess the sensory responses.
Imaging and Laboratory Tests
Additional tests may be ordered to confirm the diagnosis and identify potential underlying causes of glossopharyngeal nerve damage. Imaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT), can provide detailed images of the brain, head, and neck region. These scans can reveal any structural abnormalities, tumors, or signs of inflammation.
During an MRI or CT scan, the individual will lie on a table that slides into a large, tunnel-like machine. The machine uses a magnetic field or X-rays to create detailed images of the internal structures. The individual may need to remain still during the scan to ensure clear and accurate images. The healthcare provider will carefully analyze the images to look for any abnormalities that may be affecting the glossopharyngeal nerve.
In addition to imaging tests, laboratory tests may also be conducted to assess general health and rule out specific medical conditions. Blood work can provide valuable information about the individual’s overall health, including any signs of infection or inflammation. Other diagnostic procedures, such as a throat culture or a biopsy, may be performed to further investigate the underlying cause of the glossopharyngeal nerve damage.
Overall, the diagnosis of glossopharyngeal nerve damage involves a comprehensive evaluation of an individual’s medical history, physical examination, and additional tests. This multi-faceted approach allows healthcare professionals to gather as much information as possible to accurately diagnose the condition and determine the most appropriate treatment plan.
Treatment Options for Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can have a significant impact on an individual’s quality of life. The management of this condition depends on the underlying cause and the severity of the symptoms. While there is no one-size-fits-all approach to treatment, there are various options available to help alleviate pain and improve functionality.
Medication and Therapy
One of the primary treatment modalities for glossopharyngeal nerve damage is medication. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help reduce inflammation and alleviate discomfort. Anticonvulsant medications may also be prescribed to manage the pain associated with glossopharyngeal neuralgia, a condition characterized by severe facial pain.
In addition to medication, therapy can play a crucial role in helping individuals regain or improve their communication and swallowing abilities. Speech therapy, for example, focuses on strengthening the muscles involved in speech production and improving articulation. Swallowing therapy, on the other hand, aims to enhance the coordination of the muscles involved in swallowing, ensuring safe and efficient swallowing function.
These therapy sessions are typically conducted by trained professionals who specialize in treating individuals with neurological conditions. They work closely with patients to develop personalized treatment plans that address their specific needs and goals.
Surgical Interventions
In cases where conservative measures are insufficient or the underlying cause of nerve damage requires intervention, surgical options may be considered. The decision to undergo surgery is typically made after a thorough evaluation of the patient’s condition and a discussion of the potential risks and benefits with a healthcare professional.
One surgical approach for glossopharyngeal nerve damage is decompression. This procedure involves relieving pressure on the nerve by removing any surrounding structures that may be compressing it. By doing so, the nerve can function more effectively, reducing pain and improving overall functionality.
In some cases, the damage to the glossopharyngeal nerve may be caused by tumors or growths. In such situations, surgical removal of these abnormal growths may be necessary to restore nerve function. This procedure requires a highly skilled surgical team and careful planning to ensure the best possible outcome.
It is important to note that surgical interventions for glossopharyngeal nerve damage are complex procedures that should only be performed by experienced surgeons. The risks and benefits of surgery should be thoroughly discussed with a healthcare professional to ensure that the potential benefits outweigh the potential risks.
In conclusion, the treatment options for glossopharyngeal nerve damage are varied and depend on the underlying cause and severity of the symptoms. Medications and therapy can help manage pain and improve functionality, while surgical interventions may be necessary in certain cases. It is crucial to work closely with healthcare professionals to develop a personalized treatment plan that addresses individual needs and goals.
Prognosis and Recovery from Glossopharyngeal Nerve Damage
Factors Influencing Recovery
The prognosis for glossopharyngeal nerve damage varies depending on the extent and cause of the injury. In cases where the nerve is mildly affected or trauma-induced inflammation resolves quickly, individuals may experience partial or complete recovery over time. However, when the damage is more severe or associated with chronic conditions, the process of recovery can be more complex and may require ongoing management.
Coping and Management Strategies
Living with glossopharyngeal nerve damage can present numerous challenges, both physical and emotional. It is crucial to work closely with healthcare professionals and specialists who can provide guidance and support. They can offer advice on dietary modifications, speech exercises, and strategies to manage pain or discomfort. Additionally, maintaining overall health through regular exercise, adequate sleep, and stress management techniques can contribute to an improved sense of well-being.
Prevention of Glossopharyngeal Nerve Damage
Safety Measures and Precautions
While it may not always be possible to prevent glossopharyngeal nerve damage entirely, certain precautions and safety measures can mitigate the risk. For instance, wearing appropriate protective gear during activities that carry a higher risk of head or neck injuries, such as contact sports or certain occupations, can help reduce the likelihood of trauma-induced nerve damage. It is also essential to exercise caution during surgical procedures involving the head and neck region by carefully selecting experienced surgeons and discussing potential risks beforehand.
Regular Health Check-ups and Monitoring
Regular health check-ups and monitoring can help identify underlying conditions or risk factors that may contribute to glossopharyngeal nerve damage. By maintaining a proactive approach to healthcare, individuals can work with their healthcare providers to manage potential risks and address emerging issues promptly.
In conclusion, glossopharyngeal nerve damage can significantly impact an individual’s quality of life, affecting various aspects of speech, swallowing, and sensation. Understanding the anatomy, causes, symptoms, diagnosis, treatment options, prognosis, and prevention measures associated with glossopharyngeal nerve damage is crucial for both healthcare professionals and individuals affected by this condition. If you experience any symptoms or have concerns about your glossopharyngeal nerve, it is essential to consult with a qualified healthcare provider to undergo a thorough assessment and receive appropriate guidance and care.