The glossopharyngeal nerve is a crucial cranial nerve that plays a significant role in various functions of the head, neck, and throat. From controlling muscles involved in swallowing and speech to providing sensation to the tongue and throat, this nerve is integral for normal functioning. However, when the glossopharyngeal nerve becomes damaged, it can have profound effects on an individual’s overall health and well-being.
Understanding the Glossopharyngeal Nerve
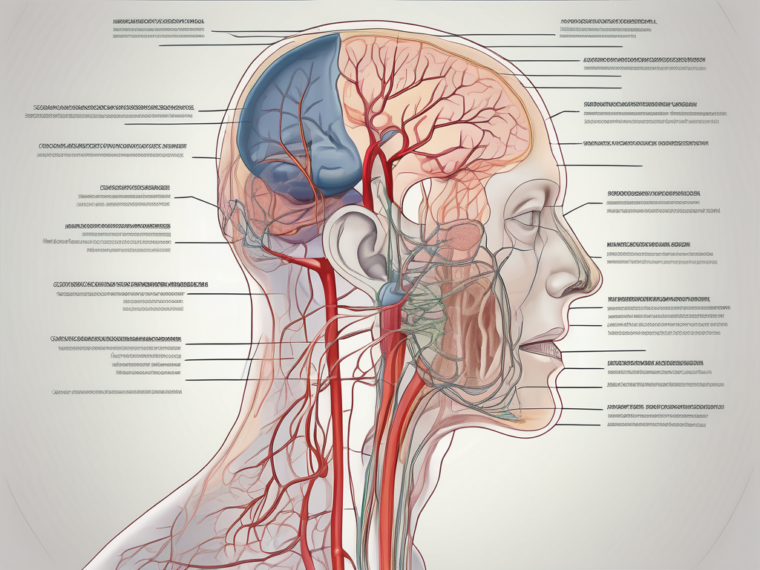
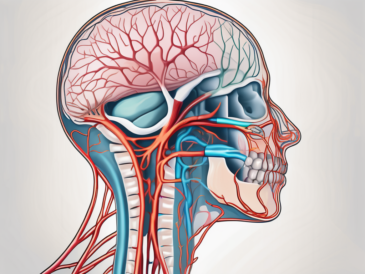
To comprehend the potential outcome of glossopharyngeal nerve damage, it is essential to first understand the anatomy and functions of this nerve. The glossopharyngeal nerve, formally known as cranial nerve IX, arises from the brainstem and consists of both motor and sensory fibers. Its anatomical pathway extends from the skull base, winding its way towards the throat, tongue, and surrounding structures.
Anatomy of the Glossopharyngeal Nerve
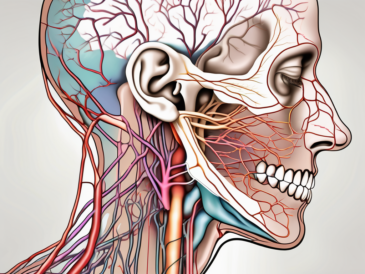
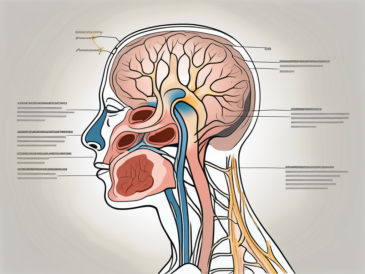
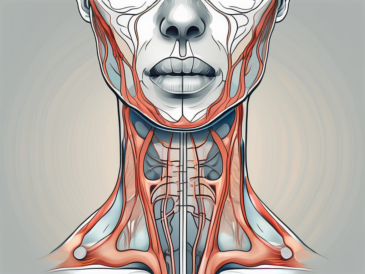
The glossopharyngeal nerve originates from the medulla oblongata, a structure in the lower part of the brainstem. Its main branches innervate the pharyngeal muscles, which are responsible for swallowing, as well as the salivary glands. Additionally, this nerve carries sensory information from the back of the throat, tongue, tonsils, and middle ear. It is through this intricate network that the glossopharyngeal nerve enables essential functions such as swallowing, taste, and even regulation of blood pressure.
The glossopharyngeal nerve’s pathway through the throat is a marvel of anatomical precision. As it winds its way from the skull base, it sends out branches to various structures along its course. These branches innervate the muscles involved in swallowing, ensuring the precise coordination required for the smooth passage of food and liquids down the esophagus. Without the glossopharyngeal nerve’s motor fibers, the act of swallowing would become a challenging and potentially dangerous task.
Furthermore, the glossopharyngeal nerve’s sensory fibers play a crucial role in our perception of taste. As they carry information from the back of the throat and tongue to the brain, they allow us to savor the flavors of our meals. Whether it’s the sweetness of a ripe strawberry or the tanginess of a lemon, the glossopharyngeal nerve enables us to experience the full range of tastes and enjoy the culinary delights of life.
But the glossopharyngeal nerve’s contributions don’t end there. It also plays a role in regulating blood pressure. Through its sensory feedback to the cardiovascular control centers in the brain, the glossopharyngeal nerve helps maintain the delicate balance of our circulatory system. By providing information about blood pressure levels, it allows the body to make necessary adjustments to keep our cardiovascular system functioning optimally.
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve serves multiple functions that significantly contribute to our daily lives. One notable function is its role in initiating the swallowing process. Imagine a scenario where a bite of food is taken, and it initiates the complex muscular coordination required for swallowing. Without the glossopharyngeal nerve’s motor fibers, this process would be severely compromised, leading to difficulties in eating and drinking.
In addition to its involvement in swallowing, the glossopharyngeal nerve also carries sensory information from the back of the throat and tongue to the brain. This sensory input contributes to our ability to taste and perceive flavors, allowing us to savor the array of tastes in our daily meals. Furthermore, the glossopharyngeal nerve plays a role in regulating blood pressure by providing sensory feedback to the cardiovascular control centers in the brain.
But the glossopharyngeal nerve’s functions extend beyond these vital roles. It also plays a part in the gag reflex, a protective mechanism that helps prevent choking. When an object or substance stimulates the back of the throat, the glossopharyngeal nerve sends signals to trigger the reflexive contraction of the muscles involved in coughing or gagging. This response helps expel potential threats and maintain the airway’s integrity.
Moreover, the glossopharyngeal nerve contributes to the sensation of pain in the throat and tongue. When these areas are injured or irritated, the nerve transmits signals to the brain, alerting us to potential problems. This pain response serves as a warning mechanism, prompting us to seek medical attention or take appropriate measures to alleviate discomfort.
Additionally, the glossopharyngeal nerve has been implicated in the regulation of saliva production. Its branches innervate the salivary glands, stimulating the secretion of saliva. This process is essential for maintaining oral health, as saliva helps lubricate the mouth, facilitate swallowing, and protect against dental decay.
In summary, the glossopharyngeal nerve is a remarkable structure with multifaceted functions. From enabling the complex coordination of swallowing to contributing to our perception of taste and regulating blood pressure, this nerve plays a vital role in our daily lives. Its intricate anatomy and diverse functions highlight the intricacies of the human body and the remarkable interplay between different systems.
Causes of Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can occur as a result of various underlying causes. Understanding these causes is crucial in identifying potential risk factors and taking appropriate preventive measures. Two primary categories that contribute to glossopharyngeal nerve damage include trauma and injuries, and medical conditions and diseases.
Trauma and Injuries
Trauma and injuries, such as head trauma or accidents involving the neck, can lead to damage to the glossopharyngeal nerve. In cases of severe trauma, the nerve may become compressed, stretched, or even torn. This can result in functional abnormalities and sensory deficits in the affected individual.
For instance, a car accident involving a sudden impact to the head or neck region can exert significant force on the glossopharyngeal nerve. The sudden jolt can cause the nerve to become compressed between bony structures, leading to injury. Additionally, sports-related injuries, such as a direct blow to the neck during contact sports like rugby or American football, can also result in glossopharyngeal nerve damage.
It is important to note that not all trauma or injuries need to be severe to cause damage to the glossopharyngeal nerve. Even minor incidents, like a fall or a sudden twist of the neck, can potentially disrupt the normal functioning of the nerve.
Medical Conditions and Diseases
Certain medical conditions and diseases can also contribute to glossopharyngeal nerve damage. These may include tumors or growths within or near the nerve, infections, such as glossopharyngeal neuralgia, or systemic diseases like diabetes or multiple sclerosis. These underlying medical conditions can disrupt the normal functioning of the nerve, leading to a range of symptoms and potential damage.
One example of a medical condition that can affect the glossopharyngeal nerve is glossopharyngeal neuralgia. This condition is characterized by severe pain in the throat, ear, and base of the tongue, which can be triggered by swallowing, speaking, or even touching the affected area. The repeated episodes of pain can put pressure on the glossopharyngeal nerve and potentially lead to damage over time.
In addition, tumors or growths within or near the glossopharyngeal nerve can exert pressure on the nerve fibers, causing compression and damage. These growths can be benign or malignant and may require surgical intervention to remove them and relieve the pressure on the nerve.
Furthermore, systemic diseases like diabetes or multiple sclerosis can also contribute to glossopharyngeal nerve damage. In diabetes, high blood sugar levels can lead to nerve damage throughout the body, including the glossopharyngeal nerve. Similarly, in multiple sclerosis, the immune system mistakenly attacks the protective covering of nerve fibers, including those of the glossopharyngeal nerve, leading to impaired function.
It is important for individuals with these medical conditions to work closely with their healthcare providers to manage their condition and minimize the risk of glossopharyngeal nerve damage.
Symptoms of Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can manifest in various ways, affecting both physical and sensory functions. Recognizing these symptoms is vital for early detection and prompt medical intervention. The symptoms can be broadly categorized as physical symptoms or sensory and motor symptoms.
Physical Symptoms
Physical symptoms of glossopharyngeal nerve damage may include difficulties in swallowing and speaking. For example, individuals may experience a sensation of food getting stuck in the throat or have a hoarse voice. Additionally, problems with controlling the muscles involved in swallowing and speech may result in voice changes or difficulties in articulation.
Swallowing difficulties can range from mild to severe, with some individuals experiencing pain or discomfort while eating or drinking. In more severe cases, complete loss of the ability to swallow may occur, requiring alternative methods of nutrition and hydration. Speech difficulties can also vary, with some individuals experiencing slurred speech or difficulty pronouncing certain sounds.
In addition to swallowing and speech issues, glossopharyngeal nerve damage can also lead to problems with facial movements. Some individuals may experience weakness or paralysis on one side of the face, making it difficult to smile, blink, or make other facial expressions. This can have a significant impact on a person’s ability to communicate nonverbally and may affect their self-esteem and emotional well-being.
Sensory and Motor Symptoms
Sensory and motor symptoms can also indicate glossopharyngeal nerve damage. These may include a decreased sense of taste or altered taste sensations, particularly at the back of the throat. Some individuals may find that certain foods taste differently or lose their enjoyment of eating due to the changes in taste perception.
In addition to taste changes, glossopharyngeal nerve damage can also affect the sense of touch and pain in the throat and tongue. Some individuals may experience a reduced ability to feel sensations in these areas or may have an increased sensitivity to touch or pain. This can make activities such as eating, drinking, or even speaking uncomfortable or painful.
Furthermore, glossopharyngeal nerve damage can lead to a loss of the gag reflex, which is an important protective mechanism for preventing choking. Without a functioning gag reflex, individuals may be at a higher risk of choking on food or liquids and may require special precautions when eating or drinking.
It is important to note that glossopharyngeal nerve damage can also affect other areas of the body beyond the throat and mouth. Some individuals may experience pain or numbness in the ears, neck, or back of the head. This can be a result of the nerve damage affecting the branches of the glossopharyngeal nerve that innervate these areas.
In conclusion, glossopharyngeal nerve damage can have a wide range of physical and sensory symptoms. From difficulties in swallowing and speaking to changes in taste perception and loss of the gag reflex, these symptoms can significantly impact a person’s daily life and overall well-being. Early detection and appropriate medical intervention are crucial in managing and treating glossopharyngeal nerve damage.
Diagnosing Glossopharyngeal Nerve Damage
Prompt and accurate diagnosis of glossopharyngeal nerve damage is crucial for effective management and potential recovery. The diagnosis typically involves a comprehensive evaluation that encompasses the patient’s medical history, physical examination, and diagnostic tests and procedures.
Glossopharyngeal nerve damage can have various causes, including trauma, infections, tumors, or underlying medical conditions such as diabetes or multiple sclerosis. Therefore, obtaining a detailed medical history is essential in identifying potential risk factors and understanding the context of the nerve damage.
During the medical history assessment, the healthcare provider will inquire about the individual’s symptoms, potential underlying medical conditions, and any recent trauma or injuries. They will also ask about any difficulties the patient may be experiencing with swallowing, speaking, or feeling sensations in the throat and tongue.
In addition to the medical history, a thorough physical examination is conducted to assess the motor function and sensory response associated with glossopharyngeal nerve activity. The healthcare provider will examine the patient’s throat, tongue, and surrounding structures for any signs of abnormalities or dysfunction. They may also perform tests to evaluate the patient’s ability to swallow, speak, and taste.
Diagnostic Tests and Procedures
To confirm glossopharyngeal nerve damage, various diagnostic tests and procedures may be utilized. These can range from imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, to specialized tests like electromyography (EMG) or swallowing studies.
Imaging studies, such as MRI or CT scans, can provide detailed images of the head and neck region, allowing healthcare professionals to visualize the glossopharyngeal nerve and identify any structural abnormalities or lesions that may be causing the nerve damage.
Electromyography (EMG) is a specialized test that measures the electrical activity of muscles. In the case of glossopharyngeal nerve damage, EMG can help assess the function of the muscles involved in swallowing and speaking. By inserting small electrodes into the muscles, the healthcare provider can evaluate the nerve signals and muscle responses, providing valuable information about the extent and location of the nerve damage.
Swallowing studies, also known as videofluoroscopic swallowing studies or modified barium swallow studies, are performed to evaluate the patient’s ability to swallow safely and effectively. During this procedure, the patient consumes various food and liquid consistencies mixed with a contrast agent, which allows the healthcare provider to visualize the swallowing process in real-time using X-ray or fluoroscopy. This test helps identify any abnormalities or difficulties in swallowing that may be related to glossopharyngeal nerve damage.
Overall, the diagnosis of glossopharyngeal nerve damage requires a comprehensive approach, combining the patient’s medical history, physical examination, and various diagnostic tests and procedures. This multidimensional evaluation allows healthcare professionals to accurately assess the extent and underlying causes of the nerve damage, leading to appropriate management strategies and potential recovery.
Treatment Options for Glossopharyngeal Nerve Damage
The treatment options for glossopharyngeal nerve damage aim to alleviate symptoms, improve functional abilities, and address the underlying cause, if possible. It is important to note that treatment approaches may vary depending on the severity and specific nature of the nerve damage. Treatment options can include the use of medications and various therapies, as well as surgical interventions, if necessary.
Medications and Therapies
Medications, such as pain relievers, muscle relaxants, or medications targeting specific underlying medical conditions, may be prescribed to manage symptoms or mitigate further damage. Additionally, therapies like physical therapy or speech therapy can help individuals regain strength, coordination, and improve swallowing and speech abilities.
Surgical Interventions
In severe cases or when other treatment measures have proven ineffective, surgical interventions may be considered. Surgical procedures aim to address the underlying cause of glossopharyngeal nerve damage, relieve any compression or entrapment, or repair any potential structural abnormalities. It is important that individuals discuss potential surgical options, risks, and benefits with a skilled medical professional to make informed decisions.
Prognosis and Long-Term Effects of Glossopharyngeal Nerve Damage
The prognosis for individuals with glossopharyngeal nerve damage varies depending on the severity, underlying cause, and timely intervention. Some individuals may experience a complete recovery of function, while others may require ongoing management and adaptation strategies.
Recovery Expectations
The recovery process following glossopharyngeal nerve damage can be influenced by various factors, including the extent of nerve injury, the implementation of appropriate treatment measures, and the individual’s overall health and resilience. With proper medical intervention and rehabilitation, some individuals may experience significant improvement in their symptoms over time.
Potential Complications and Risks
It is important to recognize that glossopharyngeal nerve damage can potentially lead to complications and risks. These may include difficulties in swallowing or speaking, recurrent infections, malnutrition, or aspiration pneumonia. In severe cases, ongoing care and support from healthcare professionals may be necessary to manage these complications and maximize an individual’s quality of life.
Preventing Glossopharyngeal Nerve Damage
While certain causes of glossopharyngeal nerve damage may be beyond our control, there are measures individuals can take to reduce the risk or severity of potential damage. These preventive strategies primarily revolve around lifestyle modifications, regular check-ups, and early detection of any underlying medical conditions.
Lifestyle Modifications
Maintaining a healthy lifestyle that includes regular exercise, a balanced diet, and avoiding risk factors, such as excessive alcohol consumption or smoking, can contribute to overall nerve health. Additionally, practicing safe habits when engaging in potentially high-impact activities can help minimize the risk of traumatic injuries to the neck or head region.
Regular Check-ups and Early Detection
Regular check-ups with healthcare professionals, particularly dentists, otolaryngologists, or primary care physicians, can aid in the early detection of any changes or abnormalities related to the glossopharyngeal nerve. Seeking prompt medical attention when experiencing any persistent or concerning symptoms is crucial for early intervention, diagnosis, and initiation of appropriate treatment measures.
In conclusion, damage to the glossopharyngeal nerve can have significant consequences on an individual’s ability to swallow, speak, and perceive taste sensations. Understanding the anatomy, functions, and potential outcomes of glossopharyngeal nerve damage is essential for individuals to recognize the symptoms, seek timely medical assistance, and contribute to their overall well-being. If experiencing any concerning symptoms or contemplating preventive measures, it is advisable to consult with a qualified healthcare professional for comprehensive evaluation and individualized guidance.