The glossopharyngeal nerve is a vital cranial nerve that plays a significant role in various bodily functions. It is responsible for sensory input from the tongue, throat, pharynx, and tonsils, as well as controlling certain motor functions in these regions. Damage to the glossopharyngeal nerve can have serious consequences and can significantly impact a person’s quality of life.
Understanding the Glossopharyngeal Nerve
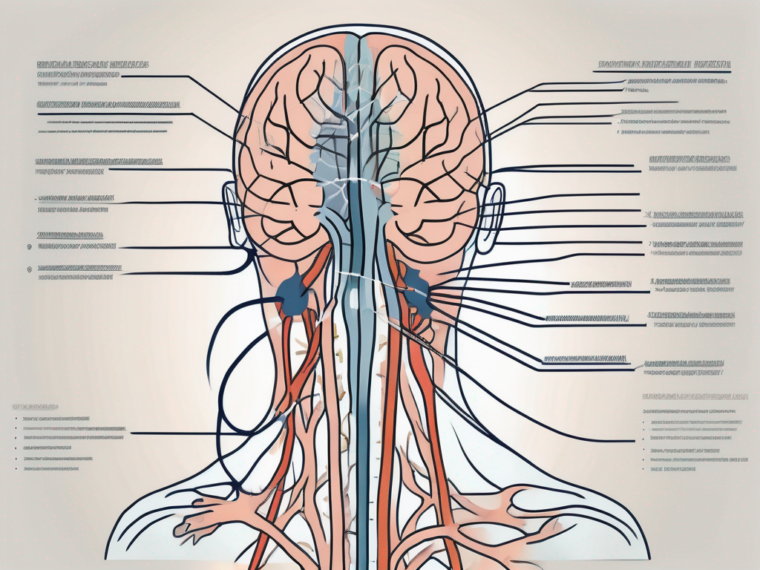
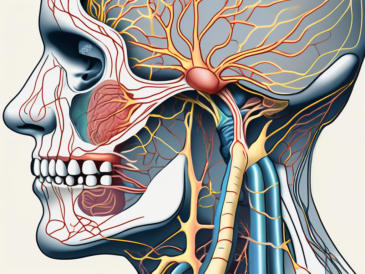
The glossopharyngeal nerve, also known as cranial nerve IX, is a crucial component of the human nervous system. It arises from the medulla oblongata, which is part of the brainstem, and extends its intricate network of sensory and motor fibers throughout the tongue and throat. This nerve is responsible for a multitude of functions, ranging from transmitting taste sensations to regulating blood pressure and heart rate.
Anatomy of the Glossopharyngeal Nerve
The glossopharyngeal nerve is a complex structure that consists of both sensory and motor fibers. The sensory fibers play a vital role in carrying information from the tongue and throat to the brain, allowing us to experience taste, touch, and pain in these areas. These fibers also contribute to the overall sensory perception of the oral cavity, enhancing our ability to appreciate the flavors and textures of the foods we consume.
On the other hand, the motor fibers of the glossopharyngeal nerve are responsible for controlling the muscles in the tongue and throat. These muscles are essential for various functions, including swallowing, speaking, and even singing. The coordinated movements of these muscles, orchestrated by the motor fibers of the glossopharyngeal nerve, enable us to articulate words and communicate effectively.
Furthermore, the glossopharyngeal nerve plays a crucial role in autonomic functions. It is involved in regulating blood pressure and heart rate, ensuring that these vital physiological processes remain within a healthy range. This nerve acts as a messenger between the brain and the cardiovascular system, constantly relaying information and making adjustments to maintain optimal cardiovascular function.
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve serves several important functions, making it an indispensable component of our daily lives. One of its primary functions is the transmission of taste sensations from the back of the tongue, throat, and tonsils. These sensory fibers allow us to savor the rich flavors of our favorite foods, enhancing our overall dining experience.
In addition to taste, the glossopharyngeal nerve also provides general sensory information from the tongue, throat, and tonsils. This includes the perception of touch and pain, enabling us to detect potential injuries or irritations in these areas. The ability to sense pain is particularly crucial as it alerts us to potential dangers and prompts us to take appropriate action to protect ourselves.
Moreover, the glossopharyngeal nerve contributes to the gag reflex, a protective mechanism that helps safeguard our airway from foreign objects. When an object stimulates the back of the throat, the sensory fibers of the glossopharyngeal nerve send signals to the brain, triggering a reflexive contraction of the throat muscles. This contraction helps expel the foreign object and prevent it from entering the respiratory system, ensuring our safety and well-being.
Overall, the glossopharyngeal nerve plays a multifaceted role in our daily lives, facilitating essential sensory and motor functions. From enabling us to taste and enjoy our favorite foods to regulating our cardiovascular system, this nerve is an integral part of our overall well-being. Understanding the anatomy and functions of the glossopharyngeal nerve allows us to appreciate the complexity and importance of this remarkable component of the human nervous system.
Causes of Glossopharyngeal Nerve Damage
The glossopharyngeal nerve is a crucial cranial nerve that plays a significant role in various functions of the head, neck, and throat region. Damage to this nerve can have debilitating effects on a person’s quality of life. While trauma and injury are primary causes of glossopharyngeal nerve damage, there are several other factors that can contribute to its impairment.
Trauma and Injury
One of the primary causes of glossopharyngeal nerve damage is trauma or injury to the head, neck, or throat region. Accidents, falls, or surgical procedures that involve these areas can result in severe damage to the nerve. Trauma can lead to compression, laceration, or stretching of the nerve, causing disruption to its normal functioning.
For instance, a severe blow to the head during a car accident can cause the glossopharyngeal nerve to become compressed between the skull and surrounding structures. This compression can impede the nerve’s ability to transmit signals effectively, leading to various symptoms such as difficulty swallowing, loss of taste sensation, and even severe pain in the throat and neck.
In addition to external trauma, internal injuries can also affect the glossopharyngeal nerve. Surgical procedures involving the head, neck, or throat region carry a risk of unintentional nerve damage. Surgeons must exercise utmost caution to minimize the risk of nerve injury during procedures such as tonsillectomy, sinus surgery, or neck dissections.
Medical Conditions and Diseases
Various medical conditions can also result in glossopharyngeal nerve damage. Tumors, infections, inflammation, or other neurological disorders can all contribute to the impairment of this vital nerve. These conditions can exert pressure on the nerve or cause inflammation in the surrounding tissues, leading to its dysfunction.
For example, glossopharyngeal neuralgia, a rare condition characterized by severe facial pain, can affect the glossopharyngeal nerve. The exact cause of this condition is unknown, but it is believed to be related to irritation or damage to the nerve. The intense pain experienced by individuals with glossopharyngeal neuralgia can significantly impact their daily lives, making it difficult to eat, speak, or even perform simple tasks.
Infections, such as tonsillitis or pharyngitis, can also lead to glossopharyngeal nerve damage. The inflammation caused by these infections can affect the nerve’s ability to transmit signals properly, resulting in symptoms like difficulty swallowing, a sensation of a lump in the throat, or even loss of taste sensation.
It is important to note that glossopharyngeal nerve damage can also occur as a secondary effect of certain systemic diseases. Conditions like diabetes, multiple sclerosis, or autoimmune disorders can cause nerve damage throughout the body, including the glossopharyngeal nerve.
Overall, glossopharyngeal nerve damage can have a profound impact on a person’s well-being. Understanding the various causes of this condition is crucial in preventing and managing its occurrence. Whether it is trauma, medical conditions, or surgical complications, taking appropriate measures to protect and preserve the glossopharyngeal nerve is essential for maintaining a healthy and functional head, neck, and throat region.
Symptoms of Glossopharyngeal Nerve Damage
Physical Symptoms
Damage to the glossopharyngeal nerve can manifest in various physical symptoms. Patients may experience difficulty swallowing, known as dysphagia, as the nerve controls the muscles involved in swallowing. This can make it challenging for individuals to consume food and liquids, leading to potential weight loss and malnutrition if not properly managed.
In addition to dysphagia, patients with glossopharyngeal nerve damage may struggle with hoarseness or loss of voice due to impaired vocal cord movements. This can impact their ability to communicate effectively, affecting both personal and professional interactions.
Furthermore, individuals with glossopharyngeal nerve damage may develop a weakened gag reflex, leading to an increased risk of choking or aspiration. This can be particularly concerning, as it can result in respiratory issues and even life-threatening complications if not addressed promptly.
Sensory Symptoms
Glossopharyngeal nerve damage can also lead to sensory symptoms. Patients may experience altered taste sensations, such as a metallic or bitter taste in the mouth. This can significantly impact their enjoyment of food and beverages, potentially leading to a decreased appetite and nutritional deficiencies.
In addition to altered taste sensations, individuals with glossopharyngeal nerve damage may have a reduced sense of taste or loss of taste altogether. This can further contribute to a diminished interest in eating and potentially result in weight loss and nutrient deficiencies.
In some cases, patients may suffer from pain or discomfort in the back of the throat or tongue. This can make it uncomfortable to eat, speak, or even swallow saliva, negatively impacting their overall quality of life.
Impact on Swallowing and Speech
Impaired swallowing and speech are common consequences of glossopharyngeal nerve damage. Patients may find it challenging to chew, swallow, or speak clearly. These difficulties can significantly impact a person’s ability to eat, communicate, and enjoy a normal, high-quality life.
Difficulties in chewing and swallowing can lead to a limited diet, as individuals may avoid certain foods that are harder to manage. This can result in a lack of variety in their meals and potential nutrient deficiencies if alternative options are not adequately explored.
The impact on speech can be equally significant, as individuals may struggle to articulate their thoughts and be understood by others. This can lead to frustration, social isolation, and difficulties in professional settings where effective communication is crucial.
Overall, glossopharyngeal nerve damage can have a profound impact on a person’s physical and sensory functions, as well as their ability to eat, speak, and enjoy life to the fullest. Proper diagnosis, treatment, and management are essential to improve quality of life and prevent further complications.
Diagnosis of Glossopharyngeal Nerve Damage
Clinical Examination
Diagnosing glossopharyngeal nerve damage begins with a thorough clinical examination. A healthcare professional will assess the patient’s symptoms, medical history, and perform physical examinations to evaluate the functioning of the affected areas. This may include testing the patient’s ability to swallow, assessing vocal cord movements, and examining the mouth and throat.
During the clinical examination, the healthcare professional may also inquire about any recent injuries or trauma to the head, neck, or throat that could potentially contribute to the nerve damage. They will carefully observe the patient’s facial expressions and listen to their speech patterns to gather additional clues about the extent and nature of the damage.
In some cases, the healthcare professional may also perform a neurological examination to assess the overall functioning of the nervous system. This may involve testing the patient’s reflexes, coordination, and sensory perception to determine if there are any other underlying neurological issues that could be contributing to the glossopharyngeal nerve damage.
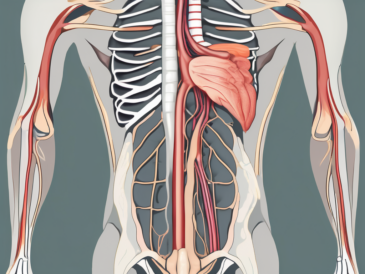
Imaging Techniques
Imaging techniques such as MRI or CT scans may be employed to visualize the structures around the glossopharyngeal nerve. These imaging studies can help identify any abnormalities or lesions that may be affecting the nerve.
During an MRI or CT scan, the patient will be positioned on a table that slides into a cylindrical machine. The machine will then use powerful magnets and radio waves to create detailed images of the structures within the body. These images can provide valuable information about the size, location, and extent of any abnormalities or lesions that may be compressing or damaging the glossopharyngeal nerve.
In some cases, a contrast dye may be injected into the patient’s bloodstream prior to the imaging study. This dye can help highlight certain structures and make them more visible on the images, allowing the healthcare professional to get a clearer view of the glossopharyngeal nerve and surrounding tissues.
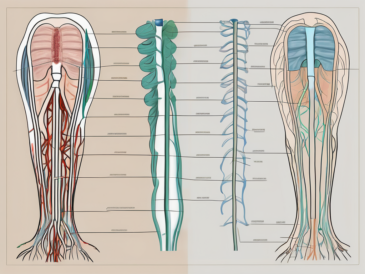
Nerve Conduction Studies
Nerve conduction studies, including electromyography (EMG), may be used to assess the electrical conduction and functioning of the glossopharyngeal nerve. These tests involve measuring the nerve’s response to electrical stimulation and can provide valuable information about the extent and location of nerve damage.
During a nerve conduction study, small electrodes are placed on the skin overlying the glossopharyngeal nerve. These electrodes deliver small electrical impulses to the nerve, and the resulting electrical activity is recorded and analyzed. By measuring the time it takes for the electrical impulses to travel along the nerve and the strength of the nerve’s response, the healthcare professional can determine if there is any damage or dysfunction present.
In addition to assessing the glossopharyngeal nerve, nerve conduction studies can also help differentiate between nerve damage and muscle weakness. By evaluating the electrical activity of the muscles innervated by the glossopharyngeal nerve, the healthcare professional can determine if the issue lies primarily with the nerve itself or if there is also muscle involvement.
Treatment Options for Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can cause a range of symptoms, including pain, difficulty swallowing, and altered taste sensations. Fortunately, there are several treatment options available to manage these symptoms and improve overall quality of life.
Medication and Drug Therapy
In some cases, medication may be prescribed to manage the symptoms associated with glossopharyngeal nerve damage. Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, can help alleviate discomfort. Anti-inflammatory drugs may also be used to reduce inflammation and swelling around the affected nerve.
Additionally, medications targeting specific symptoms, such as dysphagia (difficulty swallowing) or altered taste sensations, may be recommended. These medications can help improve swallowing function and restore a sense of taste.
It is essential for patients to consult with their healthcare provider before starting or altering any medication regimen. They can provide guidance on the appropriate dosage and potential side effects.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation can play a crucial role in improving or managing the symptoms of glossopharyngeal nerve damage. A speech-language pathologist or swallowing therapist may work with patients to develop exercises and techniques to improve swallowing, speech, and overall oral control.
These professionals can provide guidance and support in adapting to the challenges posed by glossopharyngeal nerve damage. They may recommend exercises to strengthen the muscles involved in swallowing or provide strategies to compensate for difficulties in speaking or swallowing.
Furthermore, therapists can assist patients in learning alternative methods of communication, such as using assistive devices or implementing sign language, if necessary.
Surgical Interventions
In severe cases or when conservative measures do not yield satisfactory results, surgical interventions may be considered. The specific surgical approach will depend on the underlying cause and extent of nerve damage.
Surgeons may aim to repair the damaged glossopharyngeal nerve, remove any tumors or obstructions that may be compressing the nerve, or reconstruct the affected area to restore normal function.
Prior to surgery, a thorough evaluation will be conducted to assess the feasibility and potential benefits of the procedure. The risks and potential complications will also be discussed with the patient to ensure informed decision-making.
Following surgery, a comprehensive rehabilitation program may be recommended to optimize recovery and regain functional abilities.
In conclusion, treatment options for glossopharyngeal nerve damage encompass medication and drug therapy, physical therapy and rehabilitation, as well as surgical interventions. The choice of treatment will depend on the severity of the symptoms, underlying cause, and individual patient factors. Consulting with a healthcare provider is crucial to determine the most appropriate course of action and to receive tailored care.
Prognosis and Recovery from Glossopharyngeal Nerve Damage
Factors Influencing Recovery
The prognosis and recovery from glossopharyngeal nerve damage can vary depending on several factors. The extent and location of the nerve damage, the underlying cause, and the overall health and individual circumstances of the patient can influence the recovery process. Prompt medical intervention, adherence to the prescribed treatment plan, and access to rehabilitation services are essential for optimal recovery.
Potential Complications and Challenges
Glossopharyngeal nerve damage can present various complications and challenges. For example, dysphagia can lead to malnutrition and weight loss if not adequately managed. A weakened gag reflex can increase the risk of choking or aspiration. Moreover, the impact on taste sensations can affect a person’s appetite and enjoyment of food. It is important for healthcare professionals to address these challenges and provide the necessary support and guidance for a patient’s overall well-being.
Coping and Living with Glossopharyngeal Nerve Damage
Living with glossopharyngeal nerve damage can be challenging, but it is important for patients to remember that they are not alone. Support from healthcare professionals, therapists, and support groups can provide valuable resources and assistance. Additionally, developing strategies to adapt to the effects of nerve damage, such as modifying food consistencies or using communication aids, can help individuals maintain a satisfactory quality of life. It is crucial for patients to remain engaged with their healthcare team and seek regular follow-up care as needed.
In conclusion, damage to the glossopharyngeal nerve can have significant consequences on a person’s swallowing, speech, and overall well-being. Understanding the anatomy, functions, causes, and symptoms of glossopharyngeal nerve damage is essential for accurate diagnosis and appropriate treatment. Timely intervention, comprehensive rehabilitation, and ongoing support can play a vital role in managing the effects of glossopharyngeal nerve damage and enhancing a patient’s overall quality of life. If you suspect any issues with your glossopharyngeal nerve, it is recommended to consult with a healthcare professional for a proper evaluation and guidance tailored to your specific needs.