The glossopharyngeal nerve is an important cranial nerve responsible for various functions in the head and neck region. It plays a vital role in swallowing, taste sensation, and the regulation of blood pressure. However, like any other nerve, the glossopharyngeal nerve is susceptible to damage. Understanding the causes, symptoms, diagnostic procedures, treatment options, prevention, and living with glossopharyngeal nerve damage can provide valuable insights into managing this condition effectively.
Understanding the Glossopharyngeal Nerve
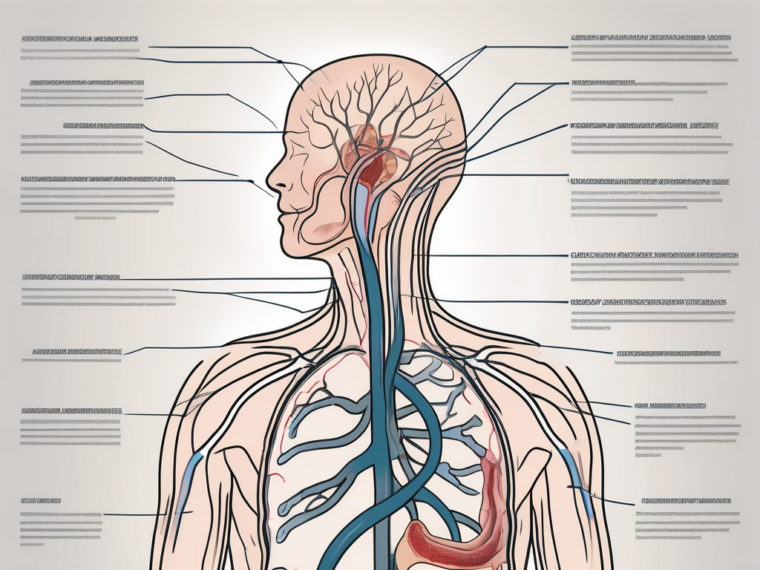
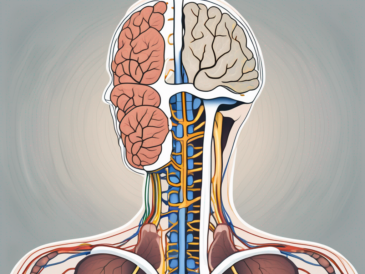
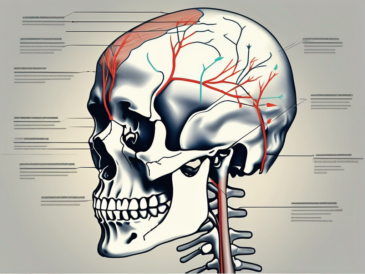
The glossopharyngeal nerve, also known as cranial nerve IX, emerges from the brainstem and supplies innervation to the back of the throat, tongue, and certain sensory organs in the head and neck. It consists of both motor and sensory fibers, making it essential for the proper functioning of various body systems.
The glossopharyngeal nerve plays a crucial role in the complex process of swallowing. When you eat or drink, the muscles involved in swallowing are activated by the motor fibers of the glossopharyngeal nerve. These muscles work together to move the food or liquid from the mouth to the esophagus, ensuring that it reaches the stomach safely.
In addition to its role in swallowing, the glossopharyngeal nerve is also responsible for the movement of the tongue. The motor fibers of the nerve innervate the muscles that allow you to move your tongue freely, enabling you to speak, taste, and manipulate food while eating.
Anatomy of the Glossopharyngeal Nerve
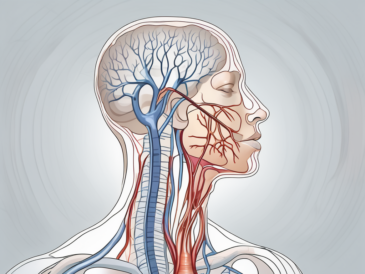
The glossopharyngeal nerve originates from the medulla oblongata, the lower part of the brainstem. It exits the skull through the jugular foramen, where it joins other cranial nerves. The nerve branches out into different structures, such as the pharynx, tongue, tonsils, and carotid sinus.
As the glossopharyngeal nerve branches out into the pharynx, it provides sensory innervation to this region. This allows you to perceive sensations such as touch, temperature, and pain in the back of your throat. It also plays a role in the gag reflex, which is a protective mechanism that helps prevent choking.
The tongue, another structure innervated by the glossopharyngeal nerve, is responsible for various functions, including taste perception. The sensory fibers of the nerve transmit taste signals from the posterior third of the tongue to the brain, allowing you to savor the flavors of different foods and beverages.
In addition to the pharynx and tongue, the glossopharyngeal nerve also supplies sensory innervation to the tonsils. This allows you to perceive sensations in this region, such as pain or discomfort, which can be indicative of infections or other underlying conditions.
Another important structure innervated by the glossopharyngeal nerve is the carotid sinus. This is a small area located in the carotid artery, which is responsible for regulating blood pressure. The sensory fibers of the glossopharyngeal nerve transmit information about blood pressure to the brain, allowing it to make necessary adjustments to maintain homeostasis.
Function of the Glossopharyngeal Nerve
The glossopharyngeal nerve has both motor and sensory functions. Motor fibers control the muscles involved in swallowing and the movement of the tongue, while sensory fibers transmit signals related to taste, touch, and pain sensations from the throat, tongue, and other regions the nerve supplies.
When it comes to taste perception, the glossopharyngeal nerve plays a significant role in transmitting signals from the posterior third of the tongue to the brain. This allows you to differentiate between different tastes, such as sweet, sour, salty, and bitter. It also contributes to the overall sensory experience of eating and drinking.
In terms of touch and pain sensations, the glossopharyngeal nerve enables you to perceive various stimuli in the back of the throat, tongue, and tonsils. This includes sensations of pressure, temperature, and discomfort, which can help alert you to potential issues or dangers in these regions.
Overall, the glossopharyngeal nerve is a vital component of the cranial nerve system, playing a crucial role in the proper functioning of the throat, tongue, and sensory organs in the head and neck. Its motor and sensory fibers work together to ensure the smooth execution of essential functions such as swallowing, taste perception, and the detection of touch and pain sensations.
Common Causes of Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can occur due to various factors. Understanding these causes can help in better prevention and management of this condition.
The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a crucial role in the functioning of the throat and tongue. It is responsible for controlling important functions such as swallowing, taste sensation in the back of the tongue, and the reflexes involved in the gag reflex.
Physical Trauma and Injuries
Direct physical trauma to the head, neck, or throat region can lead to glossopharyngeal nerve damage. This can result from falls, automobile accidents, sports-related injuries, or surgical procedures in the area.
For example, a severe blow to the head during a car accident can cause the glossopharyngeal nerve to be compressed or stretched, leading to damage. Similarly, surgical procedures involving the throat or neck area may inadvertently injure the nerve, resulting in dysfunction.
Neurological Disorders
Underlying neurological disorders like multiple sclerosis, tumors, or strokes can affect the function of the glossopharyngeal nerve. These conditions may exert pressure on the nerve or disrupt its normal signaling pathways, leading to damage.
In the case of multiple sclerosis, the immune system mistakenly attacks the protective covering of nerve fibers, including those of the glossopharyngeal nerve. This can result in nerve damage and subsequent dysfunction.
Tumors in the brain or neck region can also exert pressure on the glossopharyngeal nerve, leading to compression and damage. Similarly, strokes can cause a lack of blood flow to the nerve, resulting in ischemic damage.
Infections and Diseases
Infections, such as meningitis or abscesses in the throat, can inflame or damage the glossopharyngeal nerve. Certain systemic diseases, including diabetes or autoimmune disorders, may also contribute to nerve dysfunction and damage.
Meningitis, an infection of the membranes surrounding the brain and spinal cord, can cause inflammation in the throat area, affecting the glossopharyngeal nerve. This inflammation can lead to nerve damage and subsequent impairment of its functions.
In individuals with diabetes, high blood sugar levels can damage the blood vessels that supply the glossopharyngeal nerve, leading to nerve dysfunction. Autoimmune disorders, such as Guillain-Barré syndrome, can also result in nerve damage as the immune system mistakenly attacks the nerves.
It is important to note that glossopharyngeal nerve damage can have various symptoms, including difficulty swallowing, loss of taste sensation, and impaired gag reflex. If you experience any of these symptoms, it is essential to seek medical attention for proper diagnosis and treatment.
Symptoms of Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can manifest through various symptoms, which may vary in severity and impact on an individual’s daily life. It is important to understand these symptoms to recognize and address any potential issues.
Pain and Discomfort
One of the primary symptoms associated with glossopharyngeal nerve damage is pain in the throat, tongue, or ear region. This pain can be sharp, stabbing, or radiating, often triggered by activities like swallowing or talking. The intensity of the pain can vary from mild discomfort to severe agony, depending on the extent of the nerve damage. Consulting a healthcare professional is crucial to diagnose the underlying cause of the pain and determine appropriate treatment.
In some cases, the pain may be localized to specific areas, such as the back of the throat or the base of the tongue. This localized pain can make it difficult to eat, drink, or speak comfortably. It can also lead to sleep disturbances and affect an individual’s overall quality of life.
Furthermore, glossopharyngeal nerve damage can cause a tingling or burning sensation in the affected areas. This sensation, known as paresthesia, can be persistent or intermittent, adding to the discomfort experienced by the individual.
Swallowing Difficulties
Glossopharyngeal nerve damage can lead to swallowing difficulties, also known as dysphagia. Individuals may experience a sensation of food getting stuck in the throat or have trouble initiating the swallowing reflex. These swallowing issues may result in weight loss, malnutrition, and complications like aspiration pneumonia.
Moreover, dysphagia can significantly impact an individual’s ability to enjoy meals and maintain a healthy diet. It can cause anxiety and frustration, as every meal becomes a challenge. The fear of choking or aspirating can also lead to social isolation and a decreased quality of life.
It is important for individuals experiencing swallowing difficulties to seek medical attention promptly. A healthcare professional can evaluate the underlying cause of the dysphagia and recommend appropriate interventions, such as swallowing exercises or dietary modifications.
Voice Changes
The glossopharyngeal nerve plays a role in regulating certain muscles involved in voice production. Damage to this nerve can cause changes in voice quality, such as hoarseness or a weak voice. These voice changes can impact an individual’s ability to communicate effectively.
Hoarseness, characterized by a rough or raspy voice, can make it challenging for individuals to be understood during conversations. It can cause frustration and lead to a decreased desire to engage in social interactions. The weakness of the voice can also make it difficult to project and be heard in noisy environments.
Furthermore, individuals with glossopharyngeal nerve damage may experience vocal fatigue more quickly than before. Speaking for extended periods or at higher volumes may become exhausting, limiting their ability to participate in activities that require vocal projection, such as public speaking or singing.
Speech therapy can be beneficial for individuals with voice changes due to glossopharyngeal nerve damage. A speech-language pathologist can provide exercises and techniques to improve vocal strength and clarity, enhancing overall communication abilities.
In conclusion, glossopharyngeal nerve damage can cause a range of symptoms that can significantly impact an individual’s daily life. Pain and discomfort, swallowing difficulties, and voice changes are just a few examples of the challenges individuals may face. Seeking medical attention and exploring appropriate interventions can help manage these symptoms and improve overall well-being.
Diagnostic Procedures for Glossopharyngeal Nerve Damage
When glossopharyngeal nerve damage is suspected, several diagnostic procedures can help confirm the diagnosis and guide treatment decisions.
Glossopharyngeal nerve damage can be a complex condition, and it requires a thorough evaluation to determine the extent and underlying causes of the damage. The diagnostic process involves a combination of medical history, physical examination, and specialized tests.
Medical History and Physical Examination
A detailed medical history and physical examination are essential in evaluating glossopharyngeal nerve damage. The healthcare professional will inquire about symptoms, assess the throat and mouth, and perform neurological tests to identify any abnormalities.
During the medical history assessment, the healthcare professional will ask questions about the onset and duration of symptoms, any previous medical conditions or injuries, and any relevant family history. This information helps in understanding the potential causes and risk factors for glossopharyngeal nerve damage.
The physical examination involves a thorough examination of the throat and mouth. The healthcare professional will inspect the oral cavity, looking for any signs of inflammation, infection, or structural abnormalities. They may also perform a cranial nerve examination to assess the function of other cranial nerves that may be affected in conjunction with the glossopharyngeal nerve.
Imaging Tests
Various imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, can provide detailed images of the brain, nerves, and surrounding structures. These tests help identify any structural abnormalities or potential causes of nerve damage.
An MRI scan uses powerful magnets and radio waves to create detailed images of the brain and surrounding tissues. It can help identify any tumors, lesions, or other abnormalities that may be compressing or affecting the glossopharyngeal nerve.
A CT scan, on the other hand, uses X-rays to create cross-sectional images of the head and neck. It can provide valuable information about the bony structures and detect any fractures or abnormalities that may be contributing to the nerve damage.
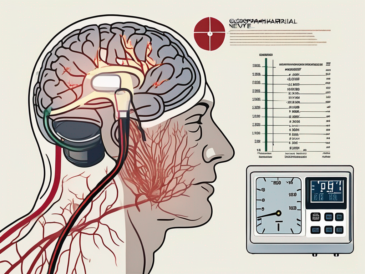
Nerve Function Tests
Electrodiagnostic tests, such as nerve conduction studies or electromyography, may be conducted to assess the function of the glossopharyngeal nerve. These tests measure the electrical activity of the nerve and help identify any abnormalities or disruptions in nerve conduction.
Nerve conduction studies involve the placement of small electrodes on the skin overlying the glossopharyngeal nerve. A small electrical impulse is then applied, and the response of the nerve is recorded. This test can help determine the speed and efficiency of nerve conduction along the glossopharyngeal nerve.
Electromyography (EMG) involves the insertion of a fine needle electrode into the muscles innervated by the glossopharyngeal nerve. The electrical activity of the muscles is then recorded during rest and contraction. This test can help identify any muscle weakness or abnormal activity associated with glossopharyngeal nerve damage.
These diagnostic procedures play a crucial role in confirming the diagnosis of glossopharyngeal nerve damage and guiding treatment decisions. By providing detailed information about the extent and underlying causes of the damage, healthcare professionals can develop an effective treatment plan tailored to the individual needs of the patient.
Treatment Options for Glossopharyngeal Nerve Damage
Treatment for glossopharyngeal nerve damage aims to alleviate symptoms, improve function, and address the underlying cause. It is crucial to consult with a healthcare professional for proper evaluation and personalized treatment recommendations.
Medications and Therapies
Depending on the underlying cause and symptoms, various medications, such as pain relievers, anticonvulsants, or muscle relaxants, may be prescribed to manage pain, reduce inflammation, or control other associated symptoms. In certain cases, physical or speech therapy may also be recommended to enhance swallow function or voice production.
Surgical Interventions
In severe cases or when conservative treatments fail to provide adequate relief, surgical interventions may be considered. Surgery aims to relieve compression on the glossopharyngeal nerve or repair any structural abnormalities contributing to nerve damage.
Lifestyle Changes and Home Remedies
While there is no specific cure for glossopharyngeal nerve damage, certain lifestyle changes and home remedies may help manage symptoms and improve overall well-being. These may include maintaining a healthy diet, practicing good oral hygiene, performing swallowing exercises, and avoiding triggers that exacerbate symptoms.
Prevention of Glossopharyngeal Nerve Damage
Although some causes of glossopharyngeal nerve damage may be unavoidable, certain preventive measures can minimize the risk and promote overall nerve health.
Regular Health Check-ups
Regular medical check-ups and screenings allow for the early detection and management of underlying conditions that may contribute to glossopharyngeal nerve damage. Routine evaluations can help identify risk factors and enable proactive interventions.
Healthy Lifestyle Practices
Maintaining a healthy lifestyle, including regular exercise, proper nutrition, and adequate rest, promotes overall nerve health. Managing chronic conditions, such as diabetes or hypertension, effectively can also reduce the risk of nerve damage and its associated complications.
Precautions for High-Risk Activities
Avoiding high-risk activities that may result in physical trauma or injury to the head and neck region can significantly reduce the risk of glossopharyngeal nerve damage. Wearing appropriate protective gear during sports or adhering to safety precautions in hazardous occupations are essential preventive measures.
Living with Glossopharyngeal Nerve Damage
Living with glossopharyngeal nerve damage can present unique challenges. However, with appropriate support and coping strategies, individuals can lead fulfilling lives.
Coping Strategies
Developing effective coping strategies can help individuals manage the physical, emotional, and social implications of glossopharyngeal nerve damage. Engaging in activities that promote relaxation, seeking support from loved ones, or joining support groups can provide a sense of empowerment and understanding.
Support Systems and Resources
Exploring available support systems and resources can provide valuable assistance to individuals living with glossopharyngeal nerve damage. Healthcare professionals, therapists, and advocacy organizations can offer information, guidance, and connect individuals with relevant services.
Long-Term Outlook and Quality of Life
The long-term outlook for individuals with glossopharyngeal nerve damage depends on various factors, such as the underlying cause, severity of symptoms, and proactive management. While complete recovery may not always be possible, timely interventions and appropriate self-care measures can help improve symptoms, enhance quality of life, and promote overall well-being.
It is important to remember that this article is for informational purposes only and should not be considered medical advice. If you suspect glossopharyngeal nerve damage or have concerns about your health, it is recommended to consult with a qualified healthcare professional for a proper evaluation and personalized recommendations.