The glossopharyngeal nerve is a vital component of the cranial nerves, responsible for carrying out various functions in the head and neck region. Understanding the role and anatomy of this important nerve is crucial for comprehending its innervation patterns and the implications of its dysfunction. In this article, we will explore in detail the anatomical structures innervated by the glossopharyngeal nerve, its clinical significance, and the treatment options for associated disorders.
Understanding the Glossopharyngeal Nerve
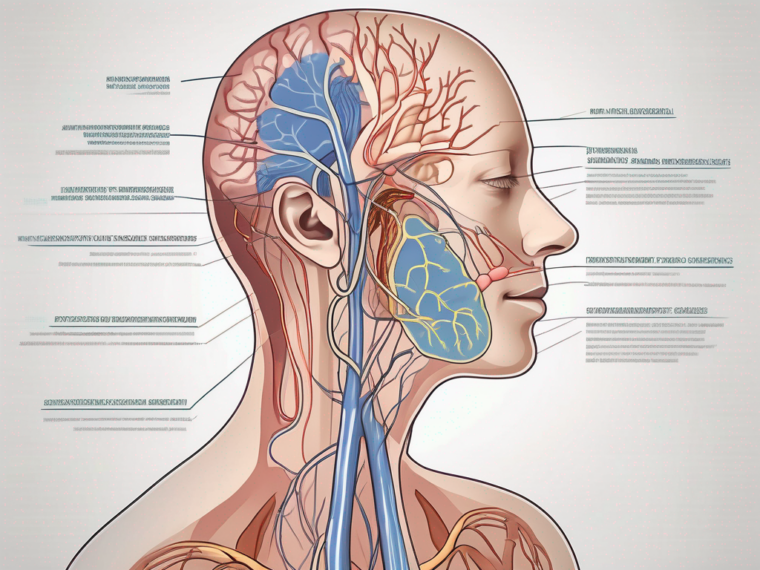
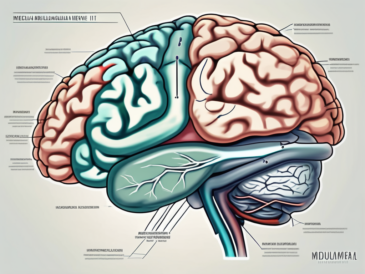
The glossopharyngeal nerve, also known as the ninth cranial nerve, emerges from the medulla oblongata, which is the lower part of the brainstem. It is primarily responsible for both motor and sensory functions in the oropharynx and surrounding structures.
The glossopharyngeal nerve plays a crucial role in the complex process of swallowing and is responsible for the coordination of multiple muscles involved in this action. It provides sensory innervation to the posterior third of the tongue, the tonsils, the oropharynx, and the soft palate.
The sensory fibers of the glossopharyngeal nerve also relay information regarding taste, touch, and proprioception from the tongue. This information is then transmitted to the central nervous system, contributing to the perception of taste and overall sensory awareness in the oral cavity.
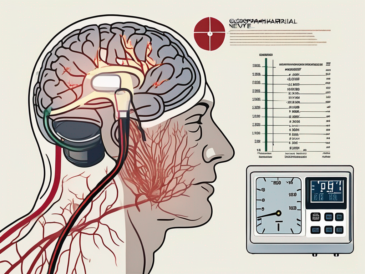
Additionally, the glossopharyngeal nerve is involved in the regulation of blood pressure and heart rate. It contains specialized sensory receptors called baroreceptors, which detect changes in blood pressure. When these receptors sense a decrease in blood pressure, they send signals to the brain, resulting in an increase in heart rate and vasoconstriction to maintain adequate blood flow.
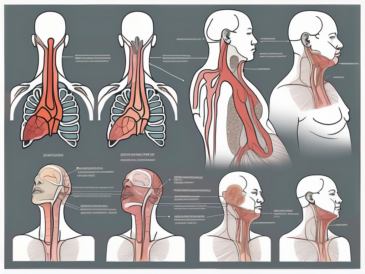
The anatomy of the glossopharyngeal nerve is fascinating. It consists of motor and sensory fibers, which originate from the glossopharyngeal nucleus in the medulla oblongata. From there, the nerve leaves the skull through the jugular foramen, a bony opening located at the base of the skull.
Once outside the skull, the glossopharyngeal nerve branches into multiple smaller nerves that innervate specific structures within the head and neck region. These branches ensure the transmission of signals and maintain the normal functioning of the innervated structures.
In addition to its role in swallowing and taste perception, the glossopharyngeal nerve also plays a part in the gag reflex. This protective reflex helps prevent choking by triggering the contraction of the muscles at the back of the throat when an object stimulates the sensory receptors in the oropharynx.
Furthermore, the glossopharyngeal nerve is involved in the regulation of salivation. It stimulates the parotid gland, the largest salivary gland, to produce saliva, which aids in the digestion of food and the lubrication of the oral cavity.
In summary, the glossopharyngeal nerve is a vital component of the nervous system, responsible for various functions related to swallowing, taste perception, blood pressure regulation, the gag reflex, and salivation. Its intricate anatomy and complex role make it an essential structure for overall oral and pharyngeal health.
Structures Innervated by the Glossopharyngeal Nerve
The glossopharyngeal nerve, also known as cranial nerve IX, plays a vital role in the innervation of several anatomical structures, including the tongue, pharynx, and parotid gland. Let’s explore each of these structures in detail.
Innervation of the Tongue
The glossopharyngeal nerve provides sensory innervation to the posterior third of the tongue, including taste buds, touch receptors, and proprioceptive fibers. This intricate network of nerve fibers enables the perception of taste, allowing us to savor the flavors of our favorite foods. Additionally, the touch receptors and proprioceptive fibers contribute to the overall sensation and control of the tongue’s movements, allowing for precise articulation of speech sounds and facilitating the process of swallowing.
When the glossopharyngeal nerve is functioning optimally, it ensures that our taste buds are able to detect the subtle nuances of flavors, enhancing our enjoyment of food. Furthermore, it plays a crucial role in maintaining the coordination and control necessary for clear and articulate speech.
Innervation of the Pharynx
The pharynx, a muscular tube responsible for swallowing and vocalization, receives both motor and sensory innervation from the glossopharyngeal nerve. Motor fibers originating from the nucleus ambiguus coordinate the muscles involved in swallowing, ensuring the smooth and efficient movement of food from the mouth to the esophagus.
On the sensory side, the glossopharyngeal nerve transmits information regarding touch, pain, and temperature from the pharynx. This sensory feedback is crucial for detecting potential dangers, such as the presence of hot or irritating substances, and triggering protective reflexes like coughing or gagging.
Damage or dysfunction of the glossopharyngeal nerve can disrupt the normal swallowing process, leading to difficulties in swallowing, a condition known as dysphagia. This can result in a range of complications, including malnutrition, dehydration, and an increased risk of aspiration pneumonia.
Innervation of the Parotid Gland
The parotid gland, one of the major salivary glands, receives parasympathetic innervation from the glossopharyngeal nerve. These parasympathetic fibers, originating from the otic ganglion, regulate salivary secretion, contributing to the maintenance of oral health and the initiation of the digestive process.
When we consume food, the glossopharyngeal nerve stimulates the parotid gland to produce saliva, which contains enzymes that aid in the breakdown of carbohydrates and facilitate the initial stages of digestion. This process not only ensures the efficient digestion of food but also helps to maintain oral hygiene by washing away food particles and preventing the buildup of harmful bacteria.
Disruption of the glossopharyngeal nerve’s function can result in decreased salivary flow, leading to xerostomia (dry mouth). This condition can have a significant impact on oral health, as the reduced saliva flow increases the risk of dental decay and gum disease. Furthermore, individuals with xerostomia may experience difficulties in swallowing and speaking, further affecting their overall quality of life.
Clinical Significance of the Glossopharyngeal Nerve
The glossopharyngeal nerve plays a crucial role in various functions of the throat and tongue, and its clinical significance cannot be overstated. Understanding the disorders and conditions that can affect this nerve is essential for early diagnosis and effective management.
Disorders Related to the Glossopharyngeal Nerve
One notable disorder associated with the glossopharyngeal nerve is glossopharyngeal neuralgia. This condition is characterized by excruciating pain in the throat, tonsils, or the base of the tongue. The pain can be triggered by seemingly simple activities such as swallowing or speaking, severely impacting an individual’s quality of life. Managing glossopharyngeal neuralgia requires a multidisciplinary approach involving neurologists, pain specialists, and sometimes even neurosurgeons.
In addition to glossopharyngeal neuralgia, other disorders can affect the glossopharyngeal nerve. Tumors compressing the nerve can lead to various symptoms and complications. These may include difficulty swallowing, changes in voice, and sensory disturbances in the tongue and throat. Infections can also impact the function of the glossopharyngeal nerve, causing similar symptoms and requiring appropriate medical intervention.
If you experience any unexplained or persistent symptoms related to the structures innervated by the glossopharyngeal nerve, it is crucial to consult with a healthcare professional for a comprehensive evaluation. An accurate diagnosis is essential for appropriate management and to rule out other potential causes.
Diagnostic Procedures for Glossopharyngeal Nerve Damage
Diagnosing glossopharyngeal nerve disorders often involves a thorough medical history review, physical examination, and specialized tests. These tests may include imaging studies, such as magnetic resonance imaging (MRI), to assess the integrity and potential compression of the nerve. MRI scans can provide detailed images of the nerve and surrounding structures, helping healthcare professionals identify any abnormalities or sources of compression.
In some cases, electromyography (EMG) may be performed to evaluate the electrical activity of the muscles innervated by the glossopharyngeal nerve. This test helps pinpoint the specific site of nerve damage and assess the severity of the condition. By analyzing the electrical signals produced by the muscles, healthcare professionals can gain valuable insights into the functioning of the glossopharyngeal nerve.
Consulting with a qualified healthcare professional is essential to determine the appropriate diagnostic approach based on individual symptoms and medical history. They will consider various factors, such as the nature and duration of symptoms, to determine the most effective diagnostic tests and develop a personalized treatment plan.
Treatment and Management of Glossopharyngeal Nerve Disorders
The treatment and management options for glossopharyngeal nerve disorders largely depend on the underlying cause and the severity of the condition. A multifaceted approach may be required to address both the symptoms and the potential cause of the nerve dysfunction.
Glossopharyngeal nerve disorders can significantly impact an individual’s quality of life, causing pain and discomfort. Therefore, it is crucial to explore various treatment options to provide relief and improve overall well-being.
Medical Interventions for Glossopharyngeal Neuralgia
For individuals diagnosed with glossopharyngeal neuralgia, various medications may be prescribed to relieve pain and reduce inflammation. These may include anticonvulsant medications to stabilize nerve activity, analgesics for pain relief, and muscle relaxants to alleviate muscle spasms that can aggravate symptoms.
Anticonvulsant medications, such as carbamazepine and gabapentin, are commonly used to manage glossopharyngeal neuralgia. These medications work by reducing the abnormal firing of nerve signals, providing relief from the sharp, shooting pain associated with the condition.
In addition to medication, lifestyle modifications can also play a significant role in managing glossopharyngeal neuralgia. Stress reduction techniques, such as meditation and yoga, can help alleviate symptoms by promoting relaxation and reducing muscle tension.
In more severe cases that do not respond well to medications, more invasive interventions, such as nerve blocks or radiofrequency ablation, may be considered. These procedures aim to disrupt the pain signals transmitted by the affected nerve fibers.
Nerve blocks involve injecting an anesthetic or a combination of anesthetic and steroid medication near the glossopharyngeal nerve to provide temporary pain relief. Radiofrequency ablation, on the other hand, uses heat generated by radio waves to destroy the problematic nerve fibers, providing long-lasting pain relief.
Surgical Options for Glossopharyngeal Nerve Damage
In cases where structural abnormalities or tumors compress the glossopharyngeal nerve, surgical intervention may be necessary to relieve the pressure and restore normal nerve function. Surgical techniques can range from decompression procedures to the complete removal of the causative factor.
Microvascular decompression is a commonly performed surgical procedure for glossopharyngeal nerve disorders. It involves identifying and gently moving blood vessels that are pressing on the nerve, thus relieving the compression and restoring normal nerve function.
Another surgical option is rhizotomy, which involves selectively cutting or ablating the glossopharyngeal nerve fibers responsible for transmitting pain signals. This procedure can provide long-term pain relief, but it may also result in some loss of sensation or taste in the affected area.
This decision is typically made by a team of specialized healthcare professionals, including neurosurgeons, depending on the individual circumstances and the expected outcomes of the procedure. They will carefully evaluate the risks and benefits of surgery and consider the patient’s overall health before proceeding with any surgical intervention.
The Glossopharyngeal Nerve in the Context of the Nervous System
The glossopharyngeal nerve does not function in isolation but rather works in close collaboration with other cranial nerves and the autonomic nervous system to maintain homeostasis and ensure proper bodily functions.
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves originating from the brainstem. It emerges from the medulla oblongata, along with other cranial nerves, and extends down into the throat and neck region. This nerve is responsible for providing both motor and sensory innervation to various structures in the head and neck.
Interactions with Other Cranial Nerves
The glossopharyngeal nerve shares connections and interacts with various cranial nerves, particularly the vagus nerve (cranial nerve X) and the accessory nerve (cranial nerve XI). These interactions allow for coordinated control over speech, swallowing, and other vital functions.
For example, the glossopharyngeal nerve and the vagus nerve work together to regulate the muscles involved in swallowing. When you swallow, the glossopharyngeal nerve sends signals to the muscles in the back of your throat, while the vagus nerve controls the muscles in your esophagus. This coordinated effort ensures that food and liquids are safely transported from your mouth to your stomach.
In addition, the glossopharyngeal nerve and the accessory nerve collaborate to control the muscles responsible for head and neck movements. This partnership allows for precise and coordinated movements, such as turning your head or shrugging your shoulders.
Understanding the complex network of cranial nerves and their interactions is crucial for healthcare professionals when assessing and diagnosing conditions affecting the glossopharyngeal nerve.
The Glossopharyngeal Nerve and the Autonomic Nervous System
In addition to its motor and sensory functions, the glossopharyngeal nerve also plays a role in the autonomic nervous system. It carries parasympathetic fibers responsible for regulating salivary secretion, blood pressure, and heart rate.
When you eat something delicious, the glossopharyngeal nerve is responsible for triggering the salivary glands to produce saliva. This saliva helps break down food and aids in the digestion process. Without the glossopharyngeal nerve’s involvement, the production of saliva would be significantly impaired.
Furthermore, the glossopharyngeal nerve contributes to the regulation of blood pressure and heart rate. It carries sensory information from the carotid sinus, a specialized area in the carotid artery that monitors blood pressure. This information is then relayed to the brain, which can initiate appropriate adjustments to maintain optimal blood pressure levels.
Disorders affecting the glossopharyngeal nerve may result in dysregulation of these autonomic functions, emphasizing the need for comprehensive evaluation and appropriate management.
In conclusion, the glossopharyngeal nerve serves an essential role in the innervation of various anatomical structures within the head and neck region. Understanding the functions, anatomy, and clinical significance of this nerve is crucial for healthcare professionals to diagnose and manage associated disorders effectively. If you have any concerns or symptoms related to the structures innervated by the glossopharyngeal nerve, it is recommended to consult with a qualified healthcare professional for a comprehensive evaluation and personalized treatment plan.