The glossopharyngeal nerve is an important cranial nerve that plays a crucial role in various bodily functions. Testing the function of this nerve is vital in diagnosing potential issues and guiding appropriate treatment strategies. In this article, we will explore the anatomy and function of the glossopharyngeal nerve, discuss the necessary preparations for the test, and delve into the step-by-step procedure of conducting the test. Additionally, we will touch on common disorders of the glossopharyngeal nerve, treatment options, and preventive measures to ensure optimal health of this important nerve.
Understanding the Glossopharyngeal Nerve
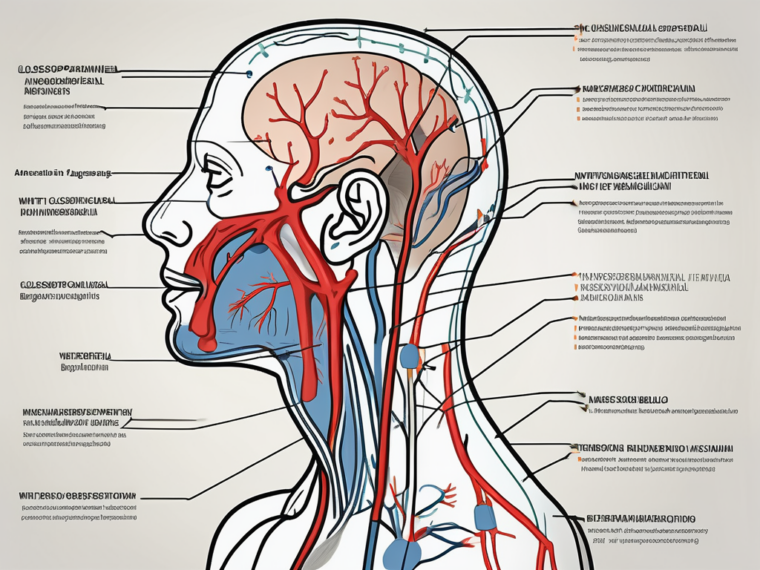
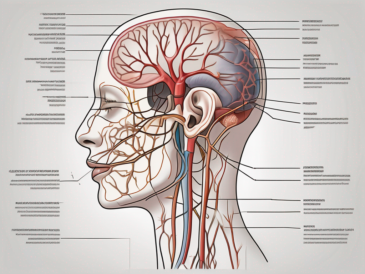
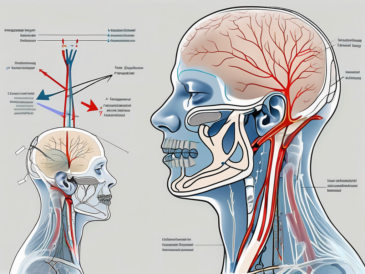
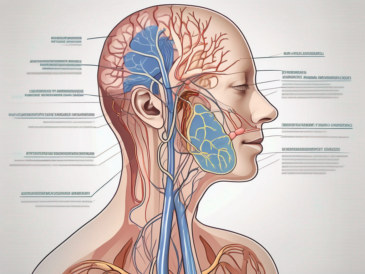
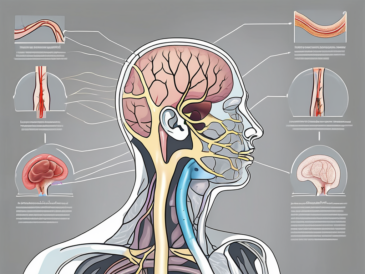
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves that emerge directly from the brain rather than the spinal cord. It originates from the medulla oblongata, the lower part of the brainstem. The nerve consists of both sensory and motor fibers, which enable it to perform its various functions throughout the body.
Anatomy of the Glossopharyngeal Nerve
The glossopharyngeal nerve is a complex structure that plays a crucial role in the functioning of the head and neck. It is composed of several branches that extend from the brainstem and innervate different regions of the body. These branches include the tympanic nerve, which supplies sensory fibers to the middle ear, and the carotid sinus nerve, which provides sensory innervation to the carotid sinus, a specialized area in the carotid artery that helps regulate blood pressure.
Additionally, the glossopharyngeal nerve gives rise to the stylopharyngeus muscle, which is responsible for elevating the pharynx during swallowing and speaking. This muscle plays a vital role in the coordination of these complex movements, ensuring efficient and effective swallowing and speech production.
Role and Function of the Glossopharyngeal Nerve
The glossopharyngeal nerve has multiple functions, including both sensory and motor functions. Sensory fibers of the glossopharyngeal nerve transmit information from the back third of the tongue, the tonsils, the throat, and parts of the ear. This information allows us to taste, swallow, and determine the position of our head and neck.
Furthermore, the glossopharyngeal nerve is involved in the regulation of blood pressure and heart rate. It carries sensory information from the carotid sinus, which monitors changes in blood pressure and relays this information to the brain. In response, the brain can initiate appropriate adjustments to maintain optimal blood pressure and heart rate.
In addition to its sensory functions, the glossopharyngeal nerve also controls the muscles needed for swallowing and speaking. Motor fibers originating from the nerve innervate the stylopharyngeus muscle, which contracts to elevate the pharynx during swallowing. This action helps propel food and liquids from the mouth to the esophagus, ensuring smooth and efficient swallowing.
Moreover, the glossopharyngeal nerve plays a role in the gag reflex, a protective mechanism that helps prevent choking. When the back of the throat is stimulated, such as by the presence of foreign objects, the glossopharyngeal nerve sends signals to the brain, triggering a reflexive response that causes the muscles in the throat to contract, expelling the potential threat.
Overall, the glossopharyngeal nerve is a vital component of the nervous system, contributing to various sensory and motor functions that are essential for proper swallowing, speech production, taste perception, and cardiovascular regulation. Its intricate anatomy and multifaceted role make it a fascinating subject of study in the field of neuroscience.
Preparing for the Glossopharyngeal Nerve Test
The glossopharyngeal nerve test is an important diagnostic procedure used to assess the function of the glossopharyngeal nerve, which is responsible for controlling various functions in the throat and tongue. Before conducting this test, it is essential to gather the necessary equipment and tools to ensure accurate and reliable results.
Necessary Equipment and Tools
When preparing for a glossopharyngeal nerve test, healthcare professionals must ensure that they have the appropriate equipment and tools at their disposal. These may include a penlight or otoscope, which are used to examine the throat and assess any abnormalities or irregularities. A spatula or tongue depressor may also be necessary to assess the movement and coordination of the tongue, as the glossopharyngeal nerve plays a crucial role in controlling these functions.
In addition to these basic tools, there may be other specialized instruments required based on the specific test being conducted. These instruments are designed to provide detailed information about the function and integrity of the glossopharyngeal nerve.
Patient Preparation Guidelines
Prior to conducting a glossopharyngeal nerve test, it is crucial to provide the patient with clear instructions and guidelines. This will ensure that the patient is well-prepared and that the test results are accurate and reliable.
One important aspect of patient preparation is informing the patient about any dietary restrictions they may need to follow before the test. Certain foods or beverages can affect the function of the glossopharyngeal nerve, so it is important for the patient to avoid consuming them for a specific period of time prior to the test.
Additionally, it is essential to inquire about any medication usage that the patient may be on. Some medications can interfere with the function of the glossopharyngeal nerve, so it is important to be aware of any potential interactions or effects that these medications may have on the test outcome.
Furthermore, it is crucial to ensure that the patient feels comfortable and understands the purpose and procedure of the glossopharyngeal nerve test. Clear communication and patient education are key in establishing trust and cooperation, which can greatly enhance the accuracy and reliability of the test results.
If necessary, healthcare professionals should consult with other healthcare professionals, such as neurologists or otolaryngologists, for further guidance and expertise in conducting the glossopharyngeal nerve test. Collaboration and interdisciplinary communication can contribute to a comprehensive and thorough assessment of the glossopharyngeal nerve function.
Conducting the Glossopharyngeal Nerve Test
The glossopharyngeal nerve test is a crucial examination that helps determine the functionality of the glossopharyngeal nerve. This nerve plays a vital role in various functions, including swallowing, taste sensation, and the gag reflex. By conducting this test, healthcare professionals can assess the nerve’s performance and identify any potential issues or abnormalities that may require further evaluation and treatment.
Step-by-Step Procedure
The glossopharyngeal nerve test typically involves a series of examinations and assessments to thoroughly evaluate the nerve’s functionality. While the specific procedures may vary depending on the suspected issue or disorder, there is a general outline that healthcare professionals follow to ensure a comprehensive evaluation.
The first step in the procedure is examining the throat. This involves a visual inspection of the oral cavity and the back of the throat to check for any visible abnormalities or signs of inflammation. Healthcare professionals may use a tongue depressor and a light source to get a clear view of the area.
Next, the healthcare professional will assess the gag reflex. This reflex is an important indicator of the glossopharyngeal nerve’s functionality. The patient will be asked to open their mouth, and the healthcare professional will gently touch the back of the throat with a cotton swab or a tongue depressor to trigger the gag reflex. The patient’s response will be observed and documented.
Another crucial aspect of the glossopharyngeal nerve test is testing taste sensations. The healthcare professional will use various substances with distinct tastes, such as sweet, sour, salty, and bitter, to evaluate the patient’s ability to perceive these tastes. This assessment helps determine if there are any abnormalities in the glossopharyngeal nerve’s ability to transmit taste signals to the brain.
Lastly, the swallowing capabilities of the patient will be evaluated. The healthcare professional may ask the patient to swallow different textures and consistencies of food or liquids while closely monitoring their ability to swallow without difficulty or discomfort. Any abnormalities or difficulties in swallowing will be noted and documented.
Throughout the entire procedure, the healthcare professional will pay careful attention to any abnormalities or variations observed. Accurate documentation of these findings is essential for the interpretation of the test results and the subsequent diagnosis and treatment plan.
Interpreting the Test Results
After conducting the glossopharyngeal nerve test, it is imperative to interpret the results accurately. This task should be performed by a qualified healthcare professional with expertise and experience in neurology. The test results provide valuable information that helps identify potential issues or abnormalities in the glossopharyngeal nerve’s functionality.
By analyzing the test results, healthcare professionals can make an accurate diagnosis and develop an appropriate treatment plan tailored to the patient’s specific needs. The interpretation of the test results may involve comparing the patient’s performance to established norms, considering the patient’s medical history, and consulting with other specialists if necessary.
It is crucial for individuals who have undergone the glossopharyngeal nerve test to consult with a healthcare provider for further evaluation and guidance. The healthcare provider will be able to provide a comprehensive analysis of the test results and recommend appropriate next steps, such as additional tests or treatments, based on the individual’s specific situation.
Overall, the glossopharyngeal nerve test is a valuable tool in assessing the functionality of this important nerve. Through a thorough and systematic evaluation, healthcare professionals can gather essential information that aids in diagnosis and treatment planning, ultimately improving the patient’s overall well-being and quality of life.
Common Disorders of the Glossopharyngeal Nerve
Glossopharyngeal Neuralgia
Glossopharyngeal neuralgia is a rare condition characterized by recurring episodes of severe pain in the throat, tongue, tonsils, and ear. These episodes can be triggered by activities such as eating, speaking, or swallowing. The pain experienced during glossopharyngeal neuralgia is often described as sharp, stabbing, or electric shock-like. It can last for a few seconds to a few minutes, and the frequency of episodes can vary from person to person.
The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a crucial role in transmitting sensory information from the back of the throat and tongue to the brain. When this nerve becomes irritated or compressed, it can result in glossopharyngeal neuralgia. The exact cause of this condition is not fully understood, but it is believed to be related to the compression of the glossopharyngeal nerve by nearby blood vessels or the presence of an abnormal growth.
While this article does not provide medical advice, it is important to consult with a medical professional if you experience any symptoms suggestive of glossopharyngeal neuralgia, as proper diagnosis and management are essential. Your healthcare provider may conduct a thorough physical examination, review your medical history, and order additional tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans to rule out other possible causes of your symptoms.
Glossopharyngeal Nerve Palsy
Glossopharyngeal nerve palsy refers to the partial or complete loss of function in the glossopharyngeal nerve. This can result in difficulty swallowing, speaking, or experiencing changes in taste. The glossopharyngeal nerve is responsible for controlling the muscles involved in swallowing and transmitting taste sensations from the back of the tongue. When this nerve is affected, it can lead to various symptoms depending on the extent of the damage.
There are several potential causes of glossopharyngeal nerve palsy, including trauma, infections, tumors, or underlying medical conditions such as diabetes or multiple sclerosis. In some cases, the exact cause may remain unknown.
If you notice any difficulty swallowing, speaking, or changes in taste, it is important to seek medical guidance for an accurate diagnosis and appropriate treatment options. A healthcare professional will be able to provide individualized recommendations based on your specific situation. Treatment for glossopharyngeal nerve palsy may involve addressing the underlying cause, managing symptoms, and providing supportive care to improve swallowing and speech abilities.
In conclusion, glossopharyngeal neuralgia and glossopharyngeal nerve palsy are two common disorders that can affect the glossopharyngeal nerve. While both conditions can cause significant discomfort and impact daily functioning, seeking medical attention is crucial for proper diagnosis and management. Remember, this article is for informational purposes only and should not replace professional medical advice.
Treatment and Management for Glossopharyngeal Nerve Disorders
Glossopharyngeal nerve disorders can be debilitating and greatly impact a person’s quality of life. Fortunately, there are various treatment options available to manage these conditions and alleviate symptoms. These treatment approaches can range from medication and non-surgical interventions to more invasive surgical procedures.
Medication and Non-Surgical Interventions
In certain cases, glossopharyngeal nerve disorders can be managed with medication and non-surgical interventions. Medications such as anticonvulsants and tricyclic antidepressants may be prescribed to alleviate pain associated with glossopharyngeal neuralgia. These medications work by targeting the underlying causes of the disorder, such as nerve irritation or abnormal signaling.
Non-surgical interventions, such as physical therapy or speech therapy, can also be effective in managing certain symptoms. Physical therapy focuses on strengthening the muscles involved in swallowing and speech, improving coordination and function. Speech therapy, on the other hand, helps individuals regain control over their speech and swallowing abilities, enhancing their overall communication skills.
It is important to note that treatment approaches should always be discussed with a healthcare professional to ensure proper guidance and supervision. Each individual’s condition is unique, and a personalized treatment plan should be developed based on their specific needs and medical history.
Surgical Treatment Options
In more severe cases or when conservative measures are ineffective, surgical treatment options may be considered. These options can include microvascular decompression, radiofrequency ablation, or surgical resection of problematic tissue.
Microvascular decompression is a surgical procedure that involves relieving pressure on the glossopharyngeal nerve by repositioning or removing blood vessels that may be compressing the nerve. This procedure aims to restore normal nerve function and alleviate pain.
Radiofrequency ablation, on the other hand, uses heat generated by radio waves to selectively destroy problematic nerve fibers. This procedure can provide long-lasting pain relief by interrupting the transmission of pain signals along the glossopharyngeal nerve.
In some cases, surgical resection of problematic tissue may be necessary. This involves removing any abnormal growths or tumors that may be causing compression or irritation of the glossopharyngeal nerve. Surgical resection is typically considered a last resort and is only performed after a thorough evaluation, proper diagnosis, and consultation with specialists in the field.
It is important to remember that surgical interventions carry risks and should only be considered after careful consideration and consultation with a healthcare professional. The decision to undergo surgery should be based on a comprehensive assessment of the individual’s condition, potential benefits, and potential risks.
In conclusion, treatment and management for glossopharyngeal nerve disorders can involve a combination of medication, non-surgical interventions, and surgical procedures. The specific approach will depend on the severity of the condition, individual needs, and consultation with healthcare professionals. With the right treatment plan, individuals with glossopharyngeal nerve disorders can experience significant improvement in their symptoms and regain a better quality of life.
Prevention and Care for Glossopharyngeal Nerve Health
Lifestyle Changes for Better Nerve Health
While it may not be possible to prevent all glossopharyngeal nerve disorders, adopting a healthy lifestyle can contribute to overall nerve health. Avoiding excessive alcohol consumption, quitting smoking, and maintaining a balanced diet rich in vitamins and minerals can support proper nerve function. Regular exercise, stress management techniques, and adequate sleep are also vital for general nerve health and well-being.
Regular Check-ups and Early Detection
Regular check-ups with a healthcare professional are essential for early detection and timely management of potential glossopharyngeal nerve disorders. Regular screenings and evaluations help identify any changes or abnormalities that may require further investigation. It is important to consult with a healthcare provider regarding the recommended frequency of check-ups based on your individual health profile.
In conclusion, testing the function of the glossopharyngeal nerve is crucial in diagnosing potential disorders and guiding appropriate treatment strategies. Understanding the anatomy, preparing for the test, and conducting the procedure accurately are all vital steps in ensuring accurate results. Additionally, being aware of common disorders, treatment options, and preventive measures can contribute to optimal glossopharyngeal nerve health. However, it is important to consult with a healthcare professional for individualized guidance and care.