The glossopharyngeal nerve holds a prominent role in the intricate world of taste perception. This crucial nerve encompasses a complex network of anatomical structures and functions. Understanding its intricate workings is key to comprehending the significant impact it has on the sense of taste. In this article, we will delve into the remarkable world of the glossopharyngeal nerve, exploring its anatomy, function, and its role in taste perception.
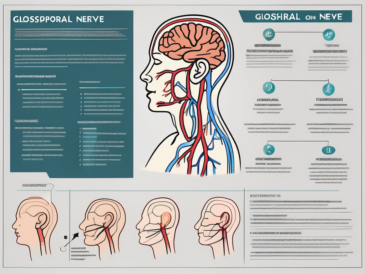
Understanding the Glossopharyngeal Nerve
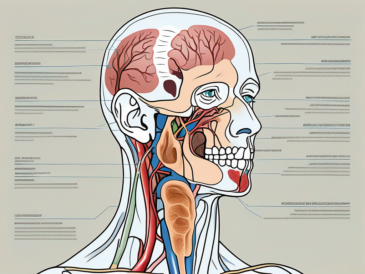
The glossopharyngeal nerve, also known as the ninth cranial nerve (CN IX), is one of the twelve cranial nerves arising from the brainstem. It emerges from the medulla oblongata, a vital region responsible for controlling various bodily functions. Acting as a two-way communication channel, the glossopharyngeal nerve receives sensory information from various regions of the head and neck and transmits motor signals to specific muscles.
The glossopharyngeal nerve is a fascinating component of the human nervous system, with a complex anatomy and a multitude of functions. Let’s delve deeper into its intricate structure and explore its role in the body.
Anatomy of the Glossopharyngeal Nerve
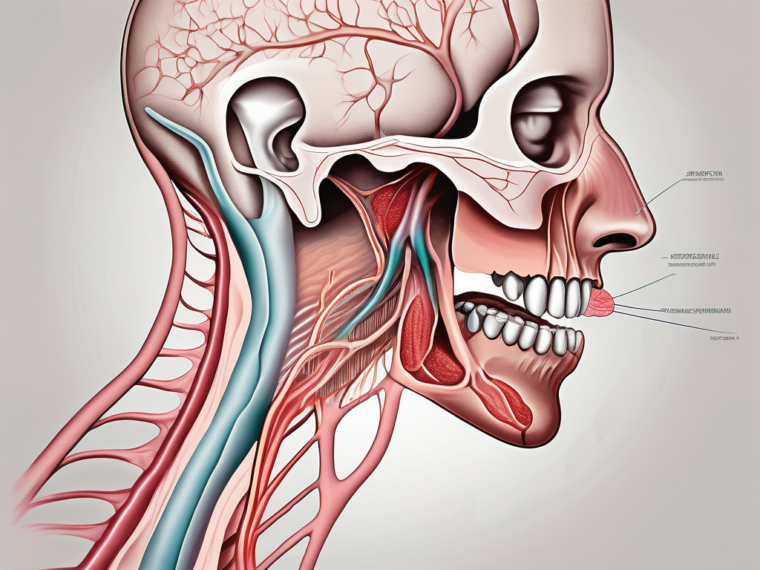
The anatomical course of the glossopharyngeal nerve begins at the base of the skull, where it arises from the medulla oblongata. From here, it travels downward, passing through several structures, including the jugular foramen and the carotid sheath. As it descends, the glossopharyngeal nerve branches out, forming connections with muscles, glands, and sensory receptors throughout its course.
One of the crucial areas of interest in the anatomy of the glossopharyngeal nerve is the posterior third of the tongue, also known as the circumvallate papillae. These papillae contain numerous taste buds, responsible for detecting different flavors. The glossopharyngeal nerve plays a pivotal role in transmitting taste signals from these taste buds to the brain for interpretation.
But the glossopharyngeal nerve’s involvement doesn’t stop there. It also innervates the stylopharyngeus muscle, which is responsible for elevating the pharynx during swallowing. This intricate connection ensures the smooth coordination of swallowing, preventing choking and facilitating the passage of food and liquids from the mouth to the esophagus.
Function of the Glossopharyngeal Nerve
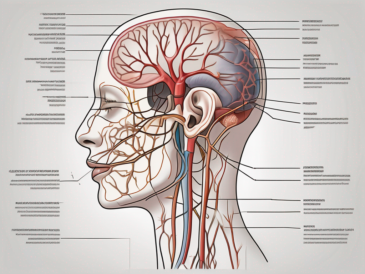
The glossopharyngeal nerve fulfills multiple functions, extending beyond taste perception alone. While its primary role involves the processing of taste signals, this remarkable nerve also contributes to other essential functions, including swallowing, salivation, and even regulation of blood pressure.
Furthermore, the glossopharyngeal nerve functions as a sensory pathway, conveying information from the pharynx, tonsils, and areas at the back of the tongue to the brain. This enables the brain to process sensations related to touch, temperature, and pain in these regions. Additionally, the glossopharyngeal nerve carries motor signals to the stylopharyngeus muscle, assisting in swallowing and speech production.
Another intriguing aspect of the glossopharyngeal nerve’s function is its involvement in the regulation of blood pressure. It contains specialized receptors called baroreceptors, which detect changes in blood pressure. When these receptors sense a decrease in blood pressure, they send signals via the glossopharyngeal nerve to the brain, triggering a series of responses aimed at restoring blood pressure to normal levels.
Moreover, the glossopharyngeal nerve plays a role in salivation, stimulating the production of saliva in the salivary glands. Saliva not only aids in the breakdown and digestion of food but also helps maintain oral health by lubricating the oral cavity and neutralizing acids that can cause tooth decay.
In conclusion, the glossopharyngeal nerve is a remarkable component of the human nervous system, with a complex anatomy and a wide range of functions. From transmitting taste signals to facilitating swallowing, salivation, and blood pressure regulation, this nerve plays a crucial role in maintaining various bodily processes. Understanding the intricacies of the glossopharyngeal nerve enhances our knowledge of the human body and highlights the remarkable interconnectedness of its systems.
The Connection Between the Glossopharyngeal Nerve and Taste
As we embark on exploring the correlation between the glossopharyngeal nerve and taste, it becomes evident that this sensory nerve heavily influences our perception of flavors.
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves originating from the brain. It emerges from the medulla oblongata, the lower part of the brainstem, and extends down the neck to innervate various structures, including the tongue, throat, and salivary glands. While it serves multiple functions, one of its crucial roles is in taste perception.
Role of the Glossopharyngeal Nerve in Taste Perception
The glossopharyngeal nerve plays a fundamental role in transmitting taste signals from specific regions of the tongue to the brain. Together with the facial nerve (CN VII) and the vagus nerve (CN X), it contributes to our comprehensive taste perception. By relaying these signals, the glossopharyngeal nerve enables the brain to distinguish and appreciate a diverse range of flavors, encompassing sweet, sour, bitter, and salty sensations.
When we consume food or drink, taste buds on the tongue detect the chemical compounds present in the substances. These taste buds are clustered in papillae, small bumps on the surface of the tongue. The glossopharyngeal nerve carries the taste information from the posterior third of the tongue, where the taste buds for bitter and sour flavors are concentrated, to the brainstem.
Once the taste signals reach the brainstem, they are further processed and transmitted to higher brain regions, such as the gustatory cortex, where the perception of taste is ultimately formed. The integration of taste information with other sensory inputs, such as smell and texture, contributes to our overall sensory experience of food and beverages.
How Damage to the Glossopharyngeal Nerve Affects Taste
Damage or dysfunction of the glossopharyngeal nerve can have a profound impact on taste perception. Individuals experiencing glossopharyngeal nerve disorders might notice alterations in their ability to discern flavors accurately. The loss of taste sensitivity, referred to as ageusia, can significantly affect one’s overall enjoyment of food and beverages.
Various factors can lead to glossopharyngeal nerve damage, including trauma, infections, tumors, or compression by adjacent structures. In some cases, the exact cause may remain unknown. Regardless of the underlying cause, it is crucial to identify and address glossopharyngeal nerve dysfunction promptly.
If you suspect any issues related to your sense of taste, it is essential to consult with a healthcare professional, preferably an otolaryngologist or a neurologist experienced in cranial nerve disorders. They can conduct a thorough evaluation, which may include physical examination, imaging studies, and specialized tests to assess the function of the glossopharyngeal nerve.
Treatment options for glossopharyngeal nerve disorders depend on the underlying cause and severity of the condition. In some cases, conservative management approaches, such as medication or physical therapy, may be sufficient to alleviate symptoms and restore taste function. However, more complex cases may require surgical interventions or other advanced treatment modalities.
It is worth noting that taste perception is a complex phenomenon influenced by various factors beyond the glossopharyngeal nerve. Factors such as age, genetics, medications, and systemic diseases can also impact our ability to taste and appreciate flavors fully.
In conclusion, the glossopharyngeal nerve plays a vital role in our ability to perceive and enjoy the diverse flavors of the world. Understanding the connection between this sensory nerve and taste can help us appreciate the intricate mechanisms underlying our sensory experiences and seek appropriate care when issues arise.
Disorders Related to the Glossopharyngeal Nerve
Despite its critical role in taste perception, the glossopharyngeal nerve is susceptible to various disorders and conditions that can impair its proper functioning. These disorders can manifest in distinct ways, each with its characteristic features and associated symptoms.
The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a crucial role in transmitting sensory information from the back of the throat, tongue, and ear to the brain. It is responsible for relaying taste sensations from the posterior third of the tongue, as well as providing sensory innervation to the pharynx and the middle ear.
Glossopharyngeal Neuralgia
Glossopharyngeal neuralgia is a rare condition characterized by recurring episodes of severe pain in the back of the throat, tongue, and ear. This condition typically arises due to irritation or compression of the glossopharyngeal nerve. The sharp, stabbing pain can be triggered by various factors, including swallowing, speaking, or even touching certain areas of the mouth.
Individuals with glossopharyngeal neuralgia often describe the pain as excruciating and debilitating, causing significant distress and impacting their quality of life. The episodes of pain can last from a few seconds to several minutes and may occur multiple times a day. In some cases, the pain can be so severe that it leads to weight loss, difficulty eating, and social isolation.
Diagnosing glossopharyngeal neuralgia can be challenging, as the symptoms can overlap with other conditions such as dental problems or temporomandibular joint disorder (TMJ). However, a thorough medical history, physical examination, and imaging studies can help in ruling out other causes and confirming the diagnosis.
Glossopharyngeal Nerve Palsy
Glossopharyngeal nerve palsy refers to a condition where there is weakness or paralysis of the muscles innervated by the glossopharyngeal nerve. This can lead to difficulties in swallowing, speech problems, and impaired taste perception. Palsy can result from various causes, including trauma, viral infections, or tumors affecting the nerve.
Individuals with glossopharyngeal nerve palsy may experience difficulty in swallowing both solids and liquids, leading to weight loss and malnutrition. Speech problems can also arise, with individuals having trouble articulating certain sounds or words. Additionally, the loss of taste sensation can affect one’s ability to enjoy food and beverages, further impacting their overall well-being.
Treatment for glossopharyngeal nerve palsy depends on the underlying cause. In some cases, conservative management, such as speech therapy and dietary modifications, may be sufficient to improve symptoms. However, in more severe cases, surgical intervention or medication may be necessary to restore proper nerve function and alleviate the associated symptoms.
Treatment and Management of Glossopharyngeal Nerve Disorders
When it comes to managing glossopharyngeal nerve disorders, a multimodal approach is often employed, tailored to the specific underlying cause and associated symptoms. Treatment options may include medication, surgical interventions, or a combination of both.
Medication Options
In cases of glossopharyngeal neuralgia, your healthcare provider may prescribe medications such as anticonvulsants or tricyclic antidepressants to help alleviate pain and reduce the frequency of episodes. Additionally, medications that target neuropathic pain, known as neuropathic pain medications, may be used to provide relief.
Anticonvulsants work by stabilizing the electrical activity in the brain, which can help reduce the abnormal firing of the glossopharyngeal nerve and subsequently alleviate pain. Tricyclic antidepressants, on the other hand, can help modulate pain signals in the brain and may be effective in managing the symptoms of glossopharyngeal neuralgia.
Neuropathic pain medications, such as gabapentin or pregabalin, target the specific mechanisms involved in neuropathic pain, providing relief by blocking the transmission of pain signals from the affected nerve fibers.
Surgical Interventions
In more severe cases or when conservative approaches prove ineffective, surgical interventions may be considered to address glossopharyngeal nerve disorders. These procedures aim to relieve compression or block pain signals by selectively damaging or severing certain nerve fibers. Surgical options may include microvascular decompression, radiofrequency thermocoagulation, or conventional ablative procedures.
Microvascular decompression involves repositioning or removing blood vessels that may be compressing the glossopharyngeal nerve. By relieving the pressure on the nerve, this procedure can help alleviate pain and other symptoms associated with glossopharyngeal nerve disorders.
Radiofrequency thermocoagulation is a minimally invasive procedure that uses heat generated by radiofrequency waves to selectively damage the nerve fibers responsible for transmitting pain signals. By interrupting the pain pathway, this procedure can provide long-lasting relief for patients with glossopharyngeal neuralgia.
Conventional ablative procedures involve the destruction of nerve fibers using various techniques, such as radiofrequency ablation, glycerol injection, or balloon compression. These procedures aim to disrupt the transmission of pain signals and can be effective in managing glossopharyngeal nerve disorders.
It is crucial to note that the decision to pursue surgical intervention should be made in close consultation with a healthcare provider experienced in the treatment of cranial nerve disorders. They will carefully evaluate the potential risks and benefits of each procedure, taking into consideration the individual patient’s condition and medical history.
The Impact of Glossopharyngeal Nerve Disorders on Quality of Life
Glossopharyngeal nerve disorders can significantly impact various aspects of an individual’s life, extending beyond somatic symptoms. The challenges they present can affect one’s physical, emotional, and social well-being.
Living with a glossopharyngeal nerve disorder can be a daily struggle, as it often leads to difficulties in basic functions such as eating and drinking. These challenges can have a profound impact on an individual’s overall quality of life, affecting not only their physical health but also their emotional and social well-being.
Challenges in Eating and Drinking
Individuals with glossopharyngeal nerve disorders may encounter difficulties in swallowing, leading to eating and drinking challenges. This can result in weight loss, malnutrition, and a decreased overall quality of life. Patients may require modifications to their diet or assistance from a speech-language pathologist to overcome these hurdles.
Imagine the frustration of not being able to enjoy a meal with family and friends, or the fear of choking every time you take a bite. These challenges can lead to feelings of isolation and sadness, as individuals with glossopharyngeal nerve disorders may find themselves avoiding social gatherings or feeling self-conscious about their eating difficulties.
Furthermore, the impact of these challenges extends beyond the physical realm. The inability to eat and drink normally can lead to a loss of pleasure and satisfaction, as food and beverages are not only a source of nourishment but also a way to connect with others and experience joy. The simple act of sharing a meal with loved ones becomes a source of frustration and sadness.
Psychological Impact of Taste Loss
The loss or alteration of taste perception can evoke emotional distress, affecting an individual’s relationship with food and the pleasure derived from eating. It is vital to address these psychological implications by seeking support from healthcare professionals or specialized therapists experienced in managing taste-related issues.
When the sense of taste is compromised, it can lead to a sense of loss and a feeling of being disconnected from the world. Food, which is often associated with comfort and enjoyment, becomes a source of disappointment and frustration. The inability to fully savor the flavors of a favorite dish or experience the pleasure of a delicious dessert can be emotionally challenging.
Moreover, the loss of taste can also impact an individual’s overall nutrition. Without the ability to fully taste and enjoy food, individuals may find it difficult to maintain a balanced diet, leading to potential nutrient deficiencies and further impacting their physical health.
Addressing the psychological impact of taste loss is crucial in improving the quality of life for individuals with glossopharyngeal nerve disorders. Seeking support from healthcare professionals who specialize in managing taste-related issues can provide valuable guidance and strategies to cope with the emotional challenges that arise.
In conclusion, glossopharyngeal nerve disorders have a significant impact on an individual’s quality of life, affecting not only their physical health but also their emotional and social well-being. The challenges in eating and drinking, as well as the psychological impact of taste loss, can create barriers to enjoying life’s simple pleasures. It is important to recognize and address these challenges to support individuals in living their lives to the fullest.
Future Research Directions in Glossopharyngeal Nerve Function
While significant progress has been made in understanding the intricate workings of the glossopharyngeal nerve, further research is required to shed light on its function fully. Ongoing investigations explore potential avenues for nerve regeneration and therapeutic approaches to address glossopharyngeal nerve disorders.
Potential for Nerve Regeneration
Emerging advancements in the field of neuroregeneration hold promise for individuals with glossopharyngeal nerve damage. Researchers are investigating various strategies, including stem cell therapy and nerve grafting techniques, which aim to restore function to damaged nerve fibers.
Advances in Treatment Approaches
Efforts are underway to develop innovative treatment approaches targeted specifically at glossopharyngeal nerve disorders. These include novel drug therapies, minimally invasive surgical techniques, and neuromodulation approaches that aim to modulate nerve activity in a more precise and targeted manner.
As the field evolves and new discoveries emerge, it is crucial to stay informed and seek expert guidance to address any concerns or disorders related to the glossopharyngeal nerve.
Conclusion
In conclusion, the glossopharyngeal nerve plays a pivotal role in taste perception and various essential functions related to the throat and tongue. Its intricate anatomy and sophisticated interconnections contribute to our comprehensive appreciation of flavors. Glossopharyngeal nerve disorders can significantly impact quality of life, warranting a multidisciplinary approach to diagnosis and management. Ongoing research and advancements offer hope for individuals affected by glossopharyngeal nerve disorders, paving the way for improved treatments and potential nerve regeneration. If you suspect any issues related to taste perception or experience symptoms associated with glossopharyngeal nerve disorders, consulting with a healthcare professional is crucial to receive appropriate guidance and care.