The glossopharyngeal nerve is a crucial component of the cranial nerves, responsible for various important functions in the human body. To evaluate the integrity and functionality of this nerve, several tests can be conducted by medical professionals. Understanding the glossopharyngeal nerve, the different tests available, interpreting test results, and treatment options for glossopharyngeal nerve damage are essential aspects to explore in order to provide a comprehensive overview of this topic.
Understanding the Glossopharyngeal Nerve
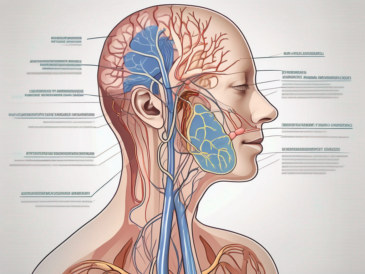
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve pairs of cranial nerves that emerge directly from the brain. It originates in the medulla oblongata, an essential part of the brainstem, and extends down through the neck before branching into various regions of the head and neck. As a mixed nerve, it contains both motor and sensory fibers, playing a vital role in both the somatic and autonomic nervous systems.
Anatomy of the Glossopharyngeal Nerve
The glossopharyngeal nerve consists of both efferent (motor) and afferent (sensory) fibers. The motor fibers innervate the stylopharyngeus muscle, which aids in swallowing and speech. This muscle is crucial for the proper movement of the pharynx during swallowing, ensuring that food and liquids are directed towards the esophagus and not the airway. The sensory fibers supply sensation to the posterior third of the tongue, allowing us to taste and appreciate a wide range of flavors. Additionally, these sensory fibers also innervate the tonsils, the soft palate, and the pharynx, providing important feedback regarding the condition and function of these structures.
The glossopharyngeal nerve’s intricate anatomy allows it to perform its various functions efficiently. The motor fibers originate in the nucleus ambiguus within the medulla oblongata and travel through the jugular foramen, a passageway located at the base of the skull. From there, they reach the stylopharyngeus muscle, enabling precise control over its movements. On the other hand, the sensory fibers arise from the superior and inferior ganglia, located near the jugular foramen. These ganglia contain the cell bodies of the sensory neurons, which receive and transmit signals from the tongue, tonsils, soft palate, and pharynx.
Functions of the Glossopharyngeal Nerve
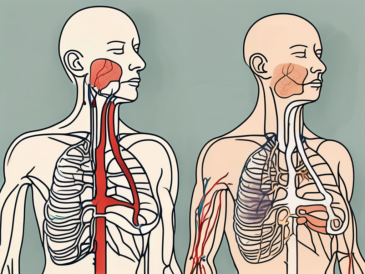
The glossopharyngeal nerve performs several important functions. It is responsible for taste perception, transmitting signals from taste buds located on the posterior third of the tongue to the brain. These taste buds detect various flavors, such as sweet, sour, bitter, and salty, allowing us to savor and enjoy different types of food. Without the glossopharyngeal nerve’s involvement, our ability to taste and appreciate the nuances of different flavors would be significantly impaired.
In addition to taste perception, the glossopharyngeal nerve also facilitates general sensation, relaying touch, pain, and temperature information from the tongue, throat, and pharynx. This sensory feedback is crucial for our ability to detect potential dangers, such as hot temperatures or sharp objects, and respond accordingly to protect ourselves. Furthermore, the glossopharyngeal nerve contributes to the regulation of blood pressure, heart rate, and respiration through its involvement in the autonomic nervous system. It carries important signals from the baroreceptors, specialized cells that detect changes in blood pressure, to the brain, allowing for appropriate adjustments to maintain cardiovascular homeostasis.
Overall, the glossopharyngeal nerve plays a multifaceted role in our daily lives, enabling us to taste, swallow, speak, and maintain vital physiological functions. Its complex anatomy and diverse functions highlight its significance in the intricate network of the cranial nerves and the overall functioning of the human body.
Different Tests for the Glossopharyngeal Nerve
To assess the function and integrity of the glossopharyngeal nerve, medical professionals may utilize various diagnostic tests. These tests help determine if the nerve is functioning properly and identify any potential issues that may be affecting its performance.
Physical Examination Techniques
During a physical examination, a doctor may evaluate the glossopharyngeal nerve by inspecting the patient’s response to stimulus. This can involve assessing the patient’s ability to taste, swallow, and articulate sounds. By observing these actions, doctors can gather valuable information about the nerve’s functionality.
In addition to these general assessments, certain neurological tests may also be performed to specifically evaluate the glossopharyngeal nerve. One such test involves touching specific areas of the tongue or throat to gauge sensation. This helps determine if the nerve is properly transmitting sensory information from these regions to the brain.
Furthermore, doctors may also examine the patient’s gag reflex, as the glossopharyngeal nerve plays a crucial role in this reflex. By testing the gag reflex, doctors can assess the nerve’s ability to initiate the appropriate response, which involves the contraction of the muscles in the back of the throat.
Imaging Tests
In some cases, imaging tests may be required to gain a better understanding of the glossopharyngeal nerve and its surrounding structures. MRI (magnetic resonance imaging) and CT (computed tomography) scans can provide detailed images of the head and neck, allowing doctors to detect any abnormalities or injuries to the nerve.
These imaging tests can reveal important information about the nerve’s anatomy, such as its location and any potential compression or damage. By visualizing the nerve and its surrounding structures, doctors can make more accurate diagnoses and develop appropriate treatment plans.
Electrical Nerve Stimulation
Electrical nerve stimulation, specifically nerve conduction studies (NCS) and electromyography (EMG), can be performed to assess the electrical activity and response of the glossopharyngeal nerve. These tests involve applying small electrical currents to specific areas and measuring the resulting nerve impulses, providing valuable information about the nerve’s functionality.
NCS measures the speed and strength of the nerve impulses as they travel along the glossopharyngeal nerve. By evaluating the conduction velocity, doctors can determine if there are any abnormalities or disruptions in the nerve’s ability to transmit electrical signals.
EMG, on the other hand, focuses on the muscles innervated by the glossopharyngeal nerve. By inserting small electrodes into the muscles, doctors can assess their electrical activity and determine if there are any issues with the nerve-muscle connection.
Both NCS and EMG are valuable tools in diagnosing conditions that affect the glossopharyngeal nerve, such as neuralgia or neuropathy. These tests provide objective data about the nerve’s functionality, helping doctors make informed decisions regarding treatment options.
Interpreting Test Results
Interpreting the results of glossopharyngeal nerve tests requires expertise and experience. Normal versus abnormal findings may vary depending on the specific diagnostic test performed and the individual being evaluated. It is of utmost importance that these tests are conducted and interpreted by qualified medical professionals who can accurately diagnose any potential issues.
When interpreting glossopharyngeal nerve test results, medical professionals carefully analyze various factors to determine the overall health and functionality of the nerve. These factors include sensory and motor functions, as well as any signs of nerve damage or dysfunction. By thoroughly evaluating these aspects, healthcare providers can gain valuable insights into the condition of the glossopharyngeal nerve and identify any potential abnormalities.
Normal vs Abnormal Findings
Normal findings during glossopharyngeal nerve testing typically include intact sensory and motor functions, with no evident signs of nerve damage or dysfunction. This indicates that the nerve is functioning optimally, allowing for proper swallowing, speech, and taste perception. However, abnormal findings may indicate various potential disorders or conditions affecting the glossopharyngeal nerve.
Abnormal test results can range from mild to severe, depending on the extent of nerve impairment. In some cases, individuals may experience partial impairment, where certain aspects of sensory or motor functions are affected. On the other hand, complete loss of function may occur, indicating a more severe condition that requires immediate attention.
When abnormal findings are present, medical professionals carefully analyze the specific nature of the impairment to determine the underlying cause. This analysis involves considering various factors such as the individual’s medical history, symptoms, and additional diagnostic tests. By thoroughly evaluating these aspects, healthcare providers can accurately diagnose the condition affecting the glossopharyngeal nerve and develop an appropriate treatment plan.
Potential Disorders and Conditions
Abnormal test results can serve as indications of underlying disorders or conditions that may affect the glossopharyngeal nerve. One potential condition is glossopharyngeal neuralgia, which is characterized by recurring episodes of severe pain in the throat, tongue, and ear. This condition can significantly impact an individual’s quality of life, making accurate diagnosis and treatment crucial.
Tumors or lesions in the area surrounding the glossopharyngeal nerve can also lead to abnormal test results. These growths can exert pressure on the nerve, causing various symptoms such as difficulty swallowing, voice changes, or pain. Early detection and intervention are essential in managing these conditions effectively.
Infections, such as glossopharyngeal cellulitis or abscesses, can also affect the glossopharyngeal nerve and produce abnormal test results. These infections can arise from bacterial or viral sources and may cause symptoms such as throat pain, difficulty speaking or swallowing, and swollen lymph nodes. Timely diagnosis and appropriate treatment are vital in preventing complications and promoting recovery.
Trauma, such as head or neck injuries, can also impact the glossopharyngeal nerve and result in abnormal test findings. The force exerted during an accident or injury can damage the nerve, leading to various symptoms such as difficulty swallowing, altered taste perception, or voice changes. Prompt medical attention is crucial in managing these cases and preventing further complications.
By identifying these conditions, medical professionals can develop appropriate treatment plans and provide the necessary support to individuals experiencing glossopharyngeal nerve-related issues. Treatment options may include medication to manage pain or inflammation, physical therapy to improve nerve function, or surgical intervention to address underlying causes such as tumors or lesions.
Treatment Options for Glossopharyngeal Nerve Damage
When glossopharyngeal nerve damage is detected, the treatment approach will depend on the underlying cause, the severity of the damage, and the individual’s overall health. Medical professionals will typically prescribe a comprehensive treatment plan that may include medication, therapies, or surgical interventions.
Glossopharyngeal nerve damage can be caused by various factors, such as trauma, infections, tumors, or underlying medical conditions like diabetes or multiple sclerosis. Identifying the root cause is crucial in determining the most effective treatment approach.
Medications play a significant role in managing the symptoms associated with glossopharyngeal nerve damage. Anticonvulsants, such as gabapentin or carbamazepine, can help reduce nerve pain and prevent seizures. Muscle relaxants like baclofen may be prescribed to alleviate muscle spasms that can affect swallowing and speech.
In addition to medication, therapies are often recommended to improve overall oral function and quality of life. Physical therapy can help strengthen the muscles involved in swallowing and improve coordination. Speech therapy focuses on enhancing speech clarity and swallowing techniques, ensuring that individuals can communicate effectively and consume food and liquids safely.
When conservative treatments fail to provide adequate relief, surgical interventions may be considered. Nerve decompression is a procedure that involves relieving pressure on the glossopharyngeal nerve by removing any compressing structures, such as blood vessels or tumors. Nerve grafting may be performed to repair damaged nerve fibers by using a healthy nerve from another part of the body as a graft. Microvascular decompression, a delicate surgical technique, aims to reposition blood vessels that are compressing the glossopharyngeal nerve, restoring its normal function.
It is important to note that the choice of treatment depends on various factors, including the individual’s overall health, the severity of the nerve damage, and the underlying cause. A multidisciplinary approach involving neurologists, otolaryngologists, and rehabilitation specialists is often necessary to develop a tailored treatment plan for each patient.
Prevention and Maintenance of Glossopharyngeal Nerve Health
The glossopharyngeal nerve is a crucial component of the nervous system that plays a vital role in various functions, including swallowing, taste sensation, and the reflexes of the throat and tongue. While it’s not always possible to prevent glossopharyngeal nerve damage, adopting a healthy lifestyle and regular medical check-ups can help maintain overall nerve health.
Lifestyle Changes
Leading a healthy lifestyle is essential for the optimal functioning of the glossopharyngeal nerve. A balanced nutrition plan that includes a variety of fruits, vegetables, whole grains, and lean proteins can provide the necessary nutrients to support nerve health. Additionally, regular exercise promotes blood circulation, which is vital for the nourishment of nerves throughout the body.
Stress management techniques, such as meditation, deep breathing exercises, and engaging in hobbies, can also contribute to the well-being of the glossopharyngeal nerve. Chronic stress can have detrimental effects on the nervous system, so finding healthy ways to cope with stress is crucial.
Avoiding trauma to the head and neck region is another important aspect of preventing glossopharyngeal nerve damage. Engaging in activities that carry a high risk of head or neck injuries, such as contact sports or extreme physical activities, should be done with caution and proper protective gear.
Practicing proper oral hygiene is not only essential for dental health but also for the well-being of the glossopharyngeal nerve. Regular brushing, flossing, and dental check-ups can help prevent infections or dental conditions that may affect the nerve’s functionality.
Minimizing alcohol and tobacco use is crucial for maintaining the health of the glossopharyngeal nerve. Excessive alcohol consumption and tobacco use have been linked to nerve damage and can increase the risk of developing nerve-related disorders.
Regular Check-ups and Monitoring
Regular check-ups with healthcare professionals are essential for monitoring the health of the glossopharyngeal nerve. Routine visits to dentists, ENT specialists, or neurologists can ensure early detection of any glossopharyngeal nerve-related issues. These healthcare professionals have the expertise to evaluate the nerve’s functionality and can recommend appropriate interventions if necessary.
During check-ups, healthcare professionals may perform various tests to evaluate the glossopharyngeal nerve’s health. These tests may include a physical examination, imaging studies, or specialized nerve function tests. Early detection of any abnormalities can lead to timely interventions and prevent further damage to the nerve.
If any concerns or symptoms related to the glossopharyngeal nerve arise, it is crucial to consult with a doctor or healthcare professional. They can provide personalized diagnosis, advice, and assistance in managing any glossopharyngeal nerve-related concerns. Self-diagnosis or relying solely on internet resources may lead to misinformation and delay appropriate treatment.
By understanding the glossopharyngeal nerve, the available tests to evaluate its functionality, and potential treatment options for glossopharyngeal nerve damage, individuals can gain insight into the importance of proper nerve health. However, it is important to note that this article provides valuable information but should not replace professional medical advice. Consulting with a qualified healthcare professional is essential for personalized diagnosis, advice, and assistance in managing any glossopharyngeal nerve-related concerns.