The glossopharyngeal nerve is a crucial component of the human nervous system that serves several essential functions. When this nerve undergoes palsy, it can potentially create a range of issues that significantly impact an individual’s overall well-being. This article aims to provide a comprehensive understanding of glossopharyngeal nerve palsy, including its anatomy, causes, symptoms, diagnosis, treatment options, and living with this condition.
Understanding the Glossopharyngeal Nerve
The glossopharyngeal nerve, also known as the ninth cranial nerve, is one of the twelve pairs of cranial nerves that originate directly from the brain. It derives its name from the Greek words “glosso,” meaning tongue, and “pharyngeal,” referring to the pharynx. This nerve is responsible for carrying sensory information from the posterior third of the tongue, tonsils, and the pharynx to the brain. Additionally, it plays a vital role in controlling various muscle functions, including swallowing and coughing.
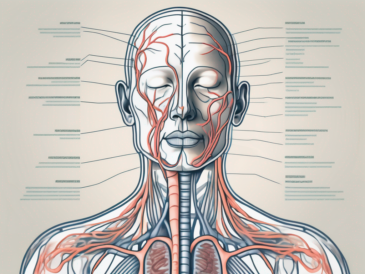
Anatomy of the Glossopharyngeal Nerve
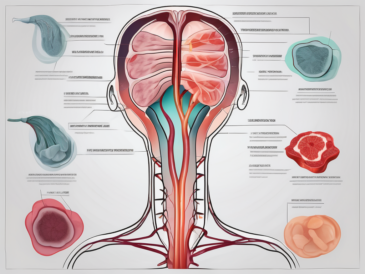
The glossopharyngeal nerve arises from the medulla oblongata, the lower part of the brainstem, and passes through several structures in the head and neck region. It consists of sensory and motor fibers, which allow for the transmission of signals between the brain and the tongue, throat, and related structures. The sensory fibers of the glossopharyngeal nerve enable taste perception, while the motor fibers regulate the movement of muscles involved in swallowing and speech.
As the glossopharyngeal nerve emerges from the brainstem, it travels through the jugular foramen, a narrow opening located at the base of the skull. Within this foramen, it is accompanied by other important structures, such as the vagus nerve and the accessory nerve. These nerves work in conjunction to ensure proper functioning of the head and neck region.
Upon exiting the jugular foramen, the glossopharyngeal nerve branches out and innervates various regions. One of its main branches, known as the tympanic nerve, provides sensory innervation to the middle ear. This allows for the perception of sound and helps maintain balance. Another significant branch, called the carotid sinus nerve, is responsible for monitoring blood pressure in the carotid sinus, a small dilation in the carotid artery.
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve performs multifaceted functions that are integral to essential bodily processes. Its sensory component facilitates tasting, general sensation, and reflexes, while the motor component serves to coordinate the muscles involved in swallowing and speech production. Moreover, the glossopharyngeal nerve also contributes to the regulation of blood pressure and respiration, demonstrating its crucial role in maintaining overall physiological balance.
When it comes to taste perception, the glossopharyngeal nerve plays a significant role in transmitting signals from the posterior third of the tongue to the brain. This allows us to differentiate between various flavors and enjoy the pleasures of eating. Additionally, the sensory fibers of the glossopharyngeal nerve provide general sensation to the tongue, tonsils, and the pharynx, allowing us to perceive touch, temperature, and pain in these regions.
The motor fibers of the glossopharyngeal nerve are responsible for coordinating the muscles involved in swallowing and speech production. These muscles work together to propel food and liquids from the mouth to the esophagus, ensuring efficient digestion. Furthermore, the glossopharyngeal nerve also plays a role in the gag reflex, a protective mechanism that helps prevent choking by triggering the contraction of the throat muscles.
Aside from its involvement in taste and motor functions, the glossopharyngeal nerve contributes to the regulation of blood pressure and respiration. It contains specialized receptors called baroreceptors, which are sensitive to changes in blood pressure. These receptors send signals to the brain, allowing it to adjust blood pressure accordingly. Additionally, the glossopharyngeal nerve also receives input from chemoreceptors, which monitor the levels of oxygen and carbon dioxide in the blood, helping to regulate respiration.
In conclusion, the glossopharyngeal nerve is a crucial component of the nervous system, responsible for carrying sensory information from the tongue, tonsils, and pharynx to the brain. It also plays a vital role in coordinating the muscles involved in swallowing and speech production. Furthermore, this nerve contributes to the regulation of blood pressure and respiration, highlighting its importance in maintaining overall physiological balance.
Causes of Glossopharyngeal Nerve Palsy
Glossopharyngeal nerve palsy can arise from various underlying causes. It is imperative to identify and address these causes to ensure appropriate management of the condition. Some possible causes include infections and trauma to the head and neck region.
Infections and Glossopharyngeal Nerve Palsy
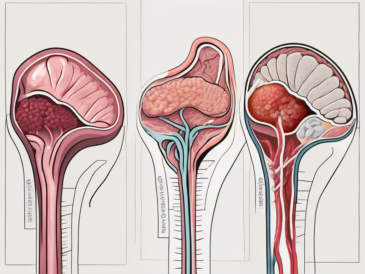
Infections, such as viral or bacterial tonsillitis, can potentially result in glossopharyngeal nerve palsy. The inflammation and swelling associated with these infections can impinge on the nerve and lead to functional impairment. In some instances, the nerve may also be affected by underlying systemic infections or inflammatory conditions, further exacerbating the symptoms of palsy.
When it comes to viral tonsillitis, the most common causative agents are the Epstein-Barr virus and the adenovirus. These viruses can invade the tonsils, causing them to become inflamed and enlarged. As a result, the glossopharyngeal nerve, which runs in close proximity to the tonsils, can be compressed or irritated, leading to palsy.
Bacterial tonsillitis, on the other hand, is often caused by Streptococcus pyogenes, commonly known as group A Streptococcus. This bacterium can cause severe inflammation of the tonsils, leading to the potential compression or irritation of the glossopharyngeal nerve.
In addition to tonsillitis, other infections such as pharyngitis, peritonsillar abscess, or even systemic infections like mononucleosis can also contribute to the development of glossopharyngeal nerve palsy. These infections can cause significant swelling and inflammation in the throat and surrounding tissues, which can affect the glossopharyngeal nerve and result in palsy.
Trauma and Glossopharyngeal Nerve Palsy
Head and neck trauma, particularly injuries that directly impact the glossopharyngeal nerve or the surrounding structures, can result in palsy. Accidents, falls, or procedures that involve surgical manipulation in the vicinity of the nerve may lead to temporary or permanent damage. It is essential to promptly seek medical attention in such cases to mitigate any potential long-term impact on nerve function.
One common cause of glossopharyngeal nerve palsy due to trauma is car accidents. The sudden impact and force exerted on the head and neck during a collision can cause injury to the glossopharyngeal nerve, resulting in palsy. Additionally, sports-related injuries, especially those involving contact sports like rugby or boxing, can also lead to trauma-induced palsy.
Surgical procedures in the head and neck region, such as tonsillectomy or neck dissection, carry a risk of glossopharyngeal nerve injury. These procedures involve delicate manipulation of tissues around the nerve, and if not performed with utmost care, can lead to nerve damage and subsequent palsy.
It is worth noting that glossopharyngeal nerve palsy can also occur spontaneously without any identifiable cause. This condition, known as idiopathic glossopharyngeal nerve palsy, presents a challenge in terms of determining the exact underlying mechanism. Further research is needed to fully understand this condition and develop appropriate treatment strategies.
Symptoms of Glossopharyngeal Nerve Palsy
Glossopharyngeal nerve palsy manifests through a variety of symptoms that can significantly affect an individual’s daily life. The symptoms may encompass physical and sensory manifestations.
Glossopharyngeal nerve palsy is a condition that affects the glossopharyngeal nerve, which is responsible for controlling various functions in the throat and tongue. When this nerve is damaged or impaired, it can lead to a range of symptoms that can have a profound impact on a person’s ability to eat, speak, and even breathe properly.
Physical Symptoms
The physical symptoms associated with glossopharyngeal nerve palsy commonly include difficulty in swallowing, leading to choking or an increased risk of aspiration. Individuals may experience hoarseness or changes in their voice quality, rendering speech challenging and strenuous. In severe cases, impaired control of the muscles involved in swallowing and coughing can lead to food or liquid entering the airway, potentially resulting in respiratory complications.
Swallowing is a complex process that involves the coordinated movement of various muscles in the throat. When the glossopharyngeal nerve is affected, these muscles may not function properly, causing difficulty in moving food from the mouth to the esophagus. This can lead to a feeling of food getting stuck in the throat, which can be distressing and uncomfortable.
Furthermore, the hoarseness and changes in voice quality that individuals with glossopharyngeal nerve palsy may experience can make communication challenging. Speaking requires precise control of the vocal cords, and when the glossopharyngeal nerve is compromised, it can affect the ability to produce clear and audible speech.
Sensory Symptoms
Glossopharyngeal nerve palsy can also lead to sensory disturbances in the posterior third of the tongue and the pharynx. This may result in altered taste perception, reduced sensitivity to touch or pain, and a diminished gag reflex. Such sensory impairments can impact an individual’s ability to appreciate certain flavors, recognize potential hazards in the oral cavity, or elicit protective reflexes when necessary.
The glossopharyngeal nerve plays a crucial role in transmitting sensory information from the tongue and pharynx to the brain. When this nerve is affected, it can disrupt the normal sensory feedback loop, leading to various sensory abnormalities. Altered taste perception can make food less enjoyable, as certain flavors may not be detected or may be perceived differently. Reduced sensitivity to touch or pain can also pose challenges, as individuals may not be able to detect potential injuries or irritations in the mouth and throat.
Additionally, a diminished gag reflex can be problematic, as it serves as a protective mechanism to prevent choking. When the glossopharyngeal nerve is impaired, the gag reflex may be weakened or absent, increasing the risk of choking on food or liquids.
In conclusion, glossopharyngeal nerve palsy can cause a range of physical and sensory symptoms that can significantly impact an individual’s quality of life. From difficulties in swallowing and speaking to altered taste perception and reduced sensory sensitivity, this condition requires proper diagnosis and management to alleviate its effects on daily functioning.
Diagnosing Glossopharyngeal Nerve Palsy
Diagnosing glossopharyngeal nerve palsy typically involves a thorough medical history evaluation and a comprehensive physical examination. Healthcare professionals may inquire about the individual’s symptoms, medical background, and potential triggers or events leading up to the onset of symptoms. The physical examination often includes an assessment of swallowing function, vocal cord movement, and sensory perception in the affected areas.
During the medical history evaluation, healthcare providers will delve into the patient’s symptoms in detail. They will ask about the nature of the symptoms, such as difficulty swallowing, hoarseness, or loss of taste sensation. Additionally, they will inquire about the duration and frequency of the symptoms, as well as any factors that seem to exacerbate or alleviate them. This information helps to paint a comprehensive picture of the patient’s condition and aids in the diagnostic process.
After gathering the necessary information from the medical history, healthcare providers proceed with a comprehensive physical examination. They will carefully observe the patient’s swallowing function, paying attention to any signs of difficulty or abnormality. This may involve asking the patient to swallow various substances, such as water or a contrast agent, while closely monitoring their ability to do so. Additionally, healthcare providers will assess vocal cord movement to determine if there is any impairment or asymmetry. They may also test the patient’s sensory perception in the affected areas, such as the back of the throat or the base of the tongue, to identify any abnormalities.
Medical History and Physical Examination
The medical history and physical examination allow healthcare providers to gather critical information that aids in the diagnosis of glossopharyngeal nerve palsy. These initial assessments help to rule out other potential causes and identify specific indicators associated with nerve dysfunction. However, further diagnostic measures may be necessary to confirm the diagnosis and determine the underlying cause.
Once the medical history and physical examination are complete, healthcare providers analyze the gathered information to form a preliminary diagnosis. They consider the patient’s symptoms, the results of the physical examination, and any relevant medical history. However, it is important to note that glossopharyngeal nerve palsy shares symptoms with other conditions, such as stroke or tumors, so further investigations are often required to confirm the diagnosis.
Imaging and Laboratory Tests
Additional investigations, such as imaging studies or laboratory tests, may be requested to support the diagnosis of glossopharyngeal nerve palsy. Imaging techniques, including magnetic resonance imaging (MRI) or computed tomography (CT), can help visualize any structural abnormalities or assess the overall condition of the nerve and surrounding structures. These imaging studies provide detailed images of the head and neck region, allowing healthcare providers to identify any potential causes of nerve dysfunction, such as tumors or nerve compression.
In some cases, healthcare providers may also recommend laboratory tests to further evaluate the patient’s condition. Blood work, for example, can help identify any underlying infections or inflammatory markers that could contribute to nerve dysfunction. By analyzing the patient’s blood samples, healthcare providers can gather valuable information about the patient’s overall health and identify any potential underlying causes of glossopharyngeal nerve palsy.
In conclusion, diagnosing glossopharyngeal nerve palsy involves a thorough medical history evaluation and a comprehensive physical examination. These initial assessments provide crucial information that aids in the diagnosis, but further investigations, such as imaging studies or laboratory tests, may be necessary to confirm the diagnosis and determine the underlying cause. By utilizing a combination of these diagnostic tools, healthcare providers can accurately diagnose glossopharyngeal nerve palsy and develop an appropriate treatment plan for the patient.
Treatment Options for Glossopharyngeal Nerve Palsy
The treatment options for glossopharyngeal nerve palsy depend on the underlying cause, severity of symptoms, and individual factors. It is crucial to consult with a medical professional to formulate an appropriate management plan.
Medications and Therapies
Medications, such as pain relievers or anti-inflammatory drugs, may be prescribed to alleviate symptoms associated with glossopharyngeal nerve palsy. In some cases, speech and swallowing therapy may also be recommended to improve muscle strength and coordination, facilitating the restoration of normal function. These therapeutic interventions can aid in minimizing the impact of palsy on an individual’s daily life and promoting optimal recovery.
Surgical Interventions
In severe cases of glossopharyngeal nerve palsy, surgical interventions may be considered. Surgical procedures aim to address any anatomical abnormalities, alleviate nerve compression or entrapment, or facilitate nerve regeneration. However, the decision to proceed with surgery is highly individualized and necessitates a comprehensive assessment of potential risks and benefits.
Living with Glossopharyngeal Nerve Palsy
Coping with glossopharyngeal nerve palsy can be challenging, both from a physical and emotional standpoint. However, with appropriate strategies and support, individuals can adapt to their circumstances and optimize their quality of life.
Coping Mechanisms and Support
Various coping mechanisms, such as modifying eating habits, practicing safe swallowing techniques, or utilizing alternative communication methods, can be employed to manage the challenges associated with glossopharyngeal nerve palsy. Seeking support from healthcare professionals, speech therapists, or support groups can provide invaluable guidance and reassurance throughout the journey of living with this condition.
Long-Term Prognosis and Quality of Life
The long-term prognosis for individuals with glossopharyngeal nerve palsy varies depending on the underlying cause, severity, and individual factors. While some cases may resolve spontaneously or respond well to conservative management, others may necessitate long-term adjustments or ongoing treatment. It is essential to work closely with healthcare professionals to ensure appropriate monitoring, management, and optimization of one’s overall well-being.
In conclusion, glossopharyngeal nerve palsy can create a range of issues that significantly impact an individual’s daily life. Understanding its anatomy, causes, symptoms, diagnosis, treatment options, and strategies for living with this condition is crucial for both affected individuals and healthcare practitioners. With prompt medical attention, appropriate management, and support, individuals can navigate the challenges posed by glossopharyngeal nerve palsy and strive for an improved quality of life. Consultation with a healthcare professional is strongly recommended for accurate diagnosis and personalized treatment plans.