The glossopharyngeal nerve, also known as the ninth cranial nerve, is a vital component of our nervous system. This article aims to explore the various aspects of this nerve, its functions, associated disorders, and potential treatments. By delving into its anatomy, role in taste sensation, involvement in swallowing and speech, regulation of blood pressure, and related disorders, we can gain a comprehensive understanding of the significant role the glossopharyngeal nerve plays in our overall well-being.
Understanding the Glossopharyngeal Nerve
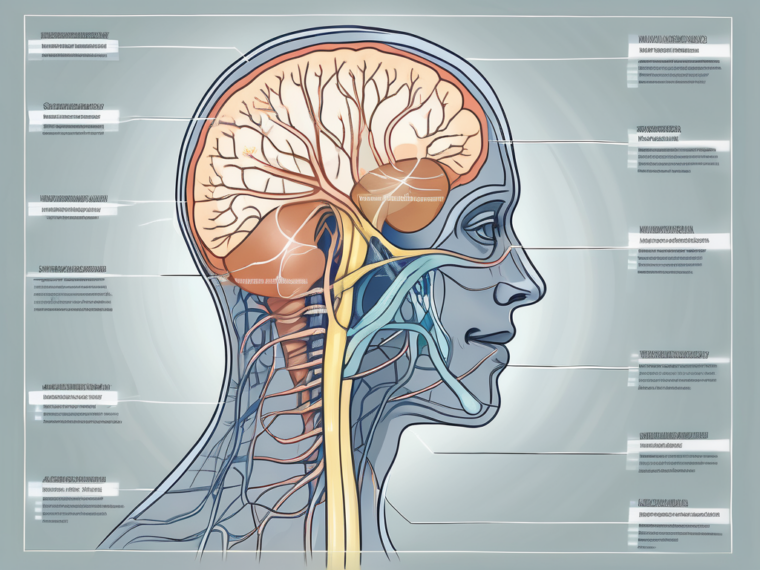
The glossopharyngeal nerve is one of the 12 pairs of cranial nerves originating from the brain. Positioned in the posterior region of the skull, it is responsible for connecting the brain to various parts of the head and neck, including the pharynx, tongue, and salivary glands. This connection ensures the proper functioning of several essential bodily processes.
The glossopharyngeal nerve, also known as cranial nerve IX, is a complex and fascinating component of the nervous system. Its intricate anatomy and connections play a vital role in maintaining the health and functionality of various bodily functions.
Anatomy of the Glossopharyngeal Nerve
To comprehend the significance of the glossopharyngeal nerve, we must first examine its intricate anatomy. This nerve emerges from the medulla oblongata, which is the lowermost portion of the brainstem. From there, it extends downward, passing through the jugular foramen before branching out to different regions.
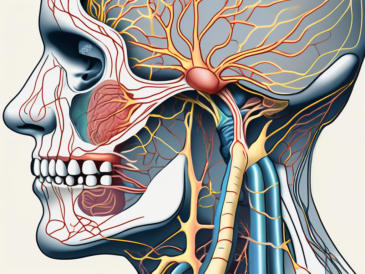
As the glossopharyngeal nerve branches out, it forms connections with various structures and tissues in the head and neck. One of its important branches is the tympanic nerve, which delivers sensory information from the middle ear. This connection allows us to perceive sounds and maintain our sense of balance.
Another significant branch of the glossopharyngeal nerve is the carotid branches. These branches are responsible for transmitting crucial information related to blood pressure regulation. Through these connections, the glossopharyngeal nerve plays a crucial role in maintaining cardiovascular health and ensuring proper blood flow to the brain.
In addition to its sensory functions, the glossopharyngeal nerve also provides innervation to the stylopharyngeus muscle located in the throat. This muscle is essential for swallowing and speech, and the glossopharyngeal nerve’s involvement in its innervation highlights its importance in facilitating these vital functions.
The Nerve’s Connection to the Brain
The glossopharyngeal nerve is intricately linked to several regions of the brain, enabling effective communication between different neural pathways. Its connection with the medulla oblongata allows the nerve to receive information from and send signals to higher brain centers involved in processing sensory input and initiating appropriate responses.
Furthermore, the glossopharyngeal nerve’s connection to the brainstem plays a crucial role in regulating autonomic functions. It is involved in controlling heart rate, blood pressure, and respiration, ensuring that these vital processes are properly regulated and coordinated.
Moreover, the glossopharyngeal nerve’s connection to the brain allows for the integration of taste sensations. It carries taste information from the posterior third of the tongue, allowing us to savor and enjoy the flavors of the food we consume.
In conclusion, the glossopharyngeal nerve is a remarkable component of the nervous system. Its intricate anatomy and connections enable it to perform a wide range of functions, from facilitating speech and swallowing to regulating cardiovascular health and integrating taste sensations. Understanding the complexity and significance of the glossopharyngeal nerve helps us appreciate the intricate workings of the human body.
Major Functions of the Glossopharyngeal Nerve
Role in Taste Sensation
One of the primary functions of the glossopharyngeal nerve is to transmit taste signals from the back of the tongue. Scientifically termed as the posterior third of the tongue, this region plays a vital role in identifying different taste qualities such as sweet, sour, salty, and bitter. The glossopharyngeal nerve relays this information to the brain, contributing to our overall sensory experience when consuming food and beverages.
The taste buds located on the posterior third of the tongue contain specialized cells called gustatory cells. These cells have tiny hair-like projections called microvilli that detect specific taste molecules. When these microvilli come into contact with taste molecules, they send signals to the glossopharyngeal nerve fibers, initiating the transmission of taste information to the brain.
Once the taste signals reach the brain, they are processed in the gustatory cortex, which is responsible for interpreting taste sensations. This complex process allows us to differentiate between various flavors and enjoy the diverse range of tastes in our favorite foods and drinks.
Its Part in Swallowing and Speech
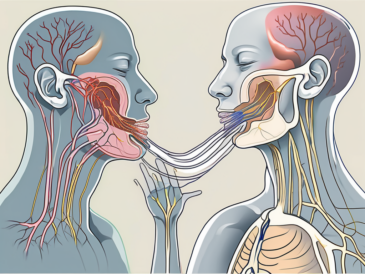
Swallowing and speaking are complex processes requiring the precise coordination of various muscles and nerves. The glossopharyngeal nerve’s involvement in these crucial functions cannot be overstated. Alongside its role in innervating the stylopharyngeus muscle, this nerve aids in the proper movement and coordination of the structures involved in swallowing and speech production. Any disruption to the glossopharyngeal nerve can significantly impact these vital functions, leading to difficulties and discomfort.
During swallowing, the glossopharyngeal nerve helps initiate the swallowing reflex by sending signals to the muscles involved in the process. These muscles, including the pharyngeal constrictor muscles and the esophageal muscles, work together to propel food or liquid from the mouth to the stomach. The glossopharyngeal nerve ensures the proper contraction and relaxation of these muscles, allowing for efficient and safe swallowing.
In addition to swallowing, the glossopharyngeal nerve also plays a crucial role in speech production. It provides sensory feedback to the brain, allowing us to monitor the position and movement of our tongue and throat muscles during speech. This feedback helps in maintaining proper articulation and pronunciation, ensuring clear and intelligible communication.
Regulation of Blood Pressure
The glossopharyngeal nerve possesses specialized receptors known as baroreceptors, which are responsible for monitoring and maintaining blood pressure. These receptors are located in the carotid sinus, a small dilation in the carotid artery. The baroreceptors detect changes in blood pressure levels and relay this information to the brain for appropriate adjustment.
When blood pressure rises, the baroreceptors in the carotid sinus send signals through the glossopharyngeal nerve to the brain, triggering a series of responses aimed at lowering blood pressure. These responses may include the dilation of blood vessels, decreased heart rate, and reduced cardiac output. Conversely, if blood pressure drops, the baroreceptors signal the brain to initiate actions that increase blood pressure, such as vasoconstriction and increased heart rate.
This intricate feedback mechanism involving the glossopharyngeal nerve helps maintain stable blood pressure levels, ensuring adequate perfusion to vital organs such as the brain, heart, and kidneys. Any dysfunction or damage to the glossopharyngeal nerve can disrupt this regulatory process, potentially leading to hypertension or hypotension.
Disorders Related to the Glossopharyngeal Nerve
Glossopharyngeal Neuralgia
Glossopharyngeal neuralgia is a condition characterized by severe, recurring pain in the throat, ear, tongue, and tonsils. It occurs due to irritation or compression of the glossopharyngeal nerve. The pain can be triggered by swallowing, talking, or even simple activities like chewing. While rare, this condition can significantly impact one’s quality of life. Any persistent or worsening symptoms should be evaluated by a medical professional to ensure appropriate diagnosis and management.
Glossopharyngeal neuralgia can be a debilitating condition, causing excruciating pain that can last for seconds to minutes. The pain is often described as sharp, stabbing, or electric shock-like. It can occur spontaneously or be triggered by various factors such as eating, drinking, coughing, or even touching the affected area. The intensity of the pain can vary from mild discomfort to severe agony, making it difficult for individuals to perform daily activities and enjoy a normal life.
Diagnosing glossopharyngeal neuralgia can be challenging as the symptoms may overlap with other conditions such as dental problems, sinusitis, or temporomandibular joint disorder. A thorough medical history, physical examination, and imaging tests may be necessary to rule out other potential causes of the symptoms. Treatment options for glossopharyngeal neuralgia include medications to manage pain, nerve blocks, and in severe cases, surgical interventions to relieve pressure on the nerve.
Implications of Damage to the Glossopharyngeal Nerve
Damage to the glossopharyngeal nerve can result from trauma, infections, tumors, or other medical conditions. Such damage can lead to a range of issues, including difficulty swallowing, impaired taste sensation, voice changes, and changes in blood pressure regulation. It is crucial to seek medical attention when experiencing any concerning symptoms or complications related to the glossopharyngeal nerve. A healthcare professional can evaluate the situation, provide an accurate diagnosis, and suggest appropriate treatment options or management strategies.
The glossopharyngeal nerve plays a vital role in various functions of the throat and mouth. When damaged, it can disrupt the coordination of muscles involved in swallowing, leading to dysphagia or difficulty swallowing. This can result in choking episodes, weight loss, and malnutrition if left untreated. Additionally, damage to the glossopharyngeal nerve can affect the taste buds located at the back of the tongue, causing a loss or alteration in taste sensation.
Furthermore, the glossopharyngeal nerve is responsible for controlling the muscles involved in vocalization. Damage to the nerve can lead to voice changes, such as hoarseness or a weak voice. This can significantly impact an individual’s ability to communicate effectively, affecting their personal and professional life. Additionally, the glossopharyngeal nerve plays a role in regulating blood pressure by monitoring oxygen and carbon dioxide levels in the blood. Damage to the nerve can disrupt this regulation, leading to fluctuations in blood pressure and potentially causing symptoms such as dizziness, fainting, or lightheadedness.
Managing the implications of glossopharyngeal nerve damage requires a multidisciplinary approach. Treatment options may include speech therapy to improve swallowing and voice function, medications to alleviate symptoms, and lifestyle modifications to manage blood pressure fluctuations. In some cases, surgical interventions may be necessary to repair or bypass the damaged nerve. Early diagnosis and intervention are crucial to prevent further complications and improve overall quality of life for individuals affected by glossopharyngeal nerve damage.
Treatment and Management of Glossopharyngeal Nerve Disorders
The glossopharyngeal nerve is a crucial component of the cranial nerves, responsible for providing sensation to the throat, tongue, and ear. When this nerve becomes damaged or compressed, it can lead to a range of disorders, including glossopharyngeal neuralgia. The treatment and management of glossopharyngeal nerve disorders aim to alleviate symptoms and improve overall quality of life.
Medical Interventions
Medical interventions play a significant role in the management of glossopharyngeal nerve disorders. One of the primary goals is to alleviate the excruciating pain associated with glossopharyngeal neuralgia. Healthcare professionals may prescribe anticonvulsant medications, such as gabapentin or carbamazepine, to help control the nerve impulses and reduce pain sensations.
In addition to pain medications, nerve blocks can also be utilized as a temporary or long-term solution. During a nerve block procedure, a local anesthetic is injected near the glossopharyngeal nerve, effectively numbing the area and providing relief from pain. This approach can be particularly beneficial for individuals who do not respond well to oral medications or those who experience severe pain episodes.
Physical therapy and speech therapy are other essential components of the treatment plan for glossopharyngeal nerve disorders. These therapies focus on addressing swallowing difficulties and speech impairments that may arise due to glossopharyngeal nerve damage. Physical therapists can guide patients through exercises and techniques to improve muscle strength and coordination, while speech therapists can help individuals regain their ability to articulate words clearly and swallow safely.
It is crucial for individuals with glossopharyngeal nerve disorders to consult with a healthcare professional to determine the most appropriate treatment plan based on their individual needs and circumstances. Each person’s experience with glossopharyngeal nerve disorders is unique, and a tailored approach is necessary to achieve optimal outcomes.
Surgical Procedures
In certain cases, surgical intervention may be necessary for the management of glossopharyngeal nerve disorders. When conservative treatments fail to provide adequate relief or when the condition significantly impacts an individual’s daily life, surgical options can be considered.
Nerve decompression is a surgical procedure that aims to relieve pressure on the glossopharyngeal nerve. During the operation, the surrounding structures that may be compressing the nerve, such as blood vessels or tumors, are carefully identified and removed. By eliminating the source of compression, this procedure can alleviate pain and other symptoms associated with glossopharyngeal nerve disorders.
Another surgical option is neurectomy, which involves the removal of a portion of the glossopharyngeal nerve. This procedure is typically reserved for individuals who have not responded well to other treatments and have persistent, debilitating symptoms. Neurectomy can provide long-term relief by interrupting the transmission of pain signals along the affected nerve.
However, the decision to proceed with surgery should be made in close consultation with medical experts. Personal circumstances, overall health, and the potential risks and benefits of the procedure must be carefully evaluated. Surgical interventions for glossopharyngeal nerve disorders are not without risks, and it is essential to weigh the potential benefits against the potential complications.
In conclusion, the treatment and management of glossopharyngeal nerve disorders involve a multidimensional approach. Medical interventions, such as pain medications and therapy, aim to alleviate symptoms and improve overall quality of life. Surgical procedures may be considered in certain cases, but careful evaluation and consultation with medical professionals are necessary to make informed decisions. With the right treatment plan, individuals with glossopharyngeal nerve disorders can find relief and regain their quality of life.
The Future of Glossopharyngeal Nerve Research
Advances in Neurological Studies
Ongoing research in the field of neurology continues to shed light on the intricacies of the glossopharyngeal nerve and its diverse functions. The glossopharyngeal nerve, also known as the ninth cranial nerve, is a crucial component of our nervous system, facilitating various essential functions. It plays a complex part in our overall well-being, from its role in taste sensation, swallowing, and speech to its involvement in regulating blood pressure.
Advancements in diagnostic techniques, such as neuroimaging, allow for more accurate assessments of the glossopharyngeal nerve and associated structures. Researchers can now visualize the nerve and its connections in greater detail, providing valuable insights into its function and potential disorders. These advancements have significantly contributed to our understanding of the glossopharyngeal nerve and its role in maintaining our overall health.
Furthermore, studies exploring the potential use of nerve stimulation and regenerative therapies show promise in improving outcomes for individuals affected by glossopharyngeal nerve disorders. Nerve stimulation techniques involve the use of electrical impulses to modulate the activity of the nerve, potentially restoring its function. Regenerative therapies, on the other hand, aim to repair or replace damaged nerve tissue, offering hope for individuals with glossopharyngeal nerve injuries or degenerative conditions.
Potential Therapeutic Approaches
As our understanding of the glossopharyngeal nerve continues to deepen, researchers are exploring innovative therapeutic approaches. Targeted drug therapies, which aim to specifically address the underlying causes of glossopharyngeal nerve disorders, are being investigated. These therapies hold the potential to provide more effective and personalized treatment options for individuals with glossopharyngeal nerve-related conditions.
In addition to drug therapies, minimally invasive interventions are being explored as potential treatment options. These procedures aim to address glossopharyngeal nerve disorders through small incisions or catheter-based techniques, minimizing the risks and recovery time associated with traditional open surgeries. Minimally invasive interventions offer the potential for improved patient outcomes and a faster return to normal daily activities.
Emerging techniques like neuromodulation are also being studied for their potential in treating glossopharyngeal nerve disorders. Neuromodulation involves the use of electrical or chemical stimulation to modulate the activity of the nerve, providing relief from symptoms and improving overall function. This approach shows promise in managing pain and other symptoms associated with glossopharyngeal nerve disorders, offering new possibilities for individuals seeking long-term relief.
However, it is important to note that these approaches are still in the experimental stages, and consultation with healthcare professionals remains paramount for comprehensive evaluation. Each individual’s condition is unique, and a personalized treatment plan should be developed in collaboration with medical experts to ensure the best possible outcomes.
In conclusion, the future holds promise for improved management and outcomes for individuals impacted by glossopharyngeal nerve-related conditions. Ongoing advancements in research, including the use of neuroimaging, nerve stimulation, regenerative therapies, targeted drug therapies, minimally invasive interventions, and neuromodulation, are expanding our understanding of the glossopharyngeal nerve and its potential therapeutic approaches. Awareness of glossopharyngeal nerve disorders and their potential implications is vital to seek appropriate medical attention and explore suitable treatment options. With continued research and potential breakthroughs, individuals affected by glossopharyngeal nerve disorders can look forward to a brighter future with improved quality of life.