Understanding the Function and Disorders of the Glossopharyngeal Nerve
The glossopharyngeal nerve is a crucial component of the human nervous system, responsible for numerous important functions related to the throat, tongue, and sensory information of the head and neck. In this article, we will provide an in-depth analysis of the anatomy, role, disorders, symptoms, diagnosis, treatment options, prevention, management, and future research directions of the glossopharyngeal nerve.
An Overview of the Glossopharyngeal Nerve
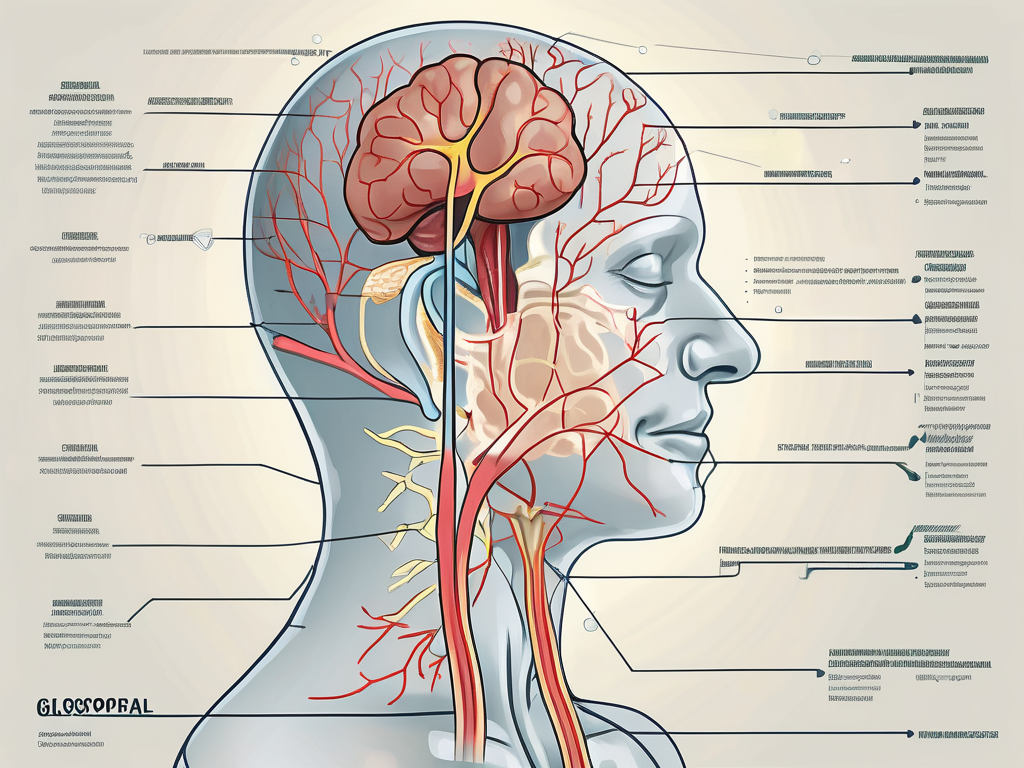
Anatomy of the Glossopharyngeal Nerve
The glossopharyngeal nerve is the ninth cranial nerve and originates from the medulla oblongata of the brainstem. It consists of both sensory and motor fibers, which perform distinct functions.
The sensory fibers of the glossopharyngeal nerve are responsible for transmitting information from the oropharynx, tonsils, posterior third of the tongue, middle ear, and other structures in the head and neck. This information is crucial for various bodily functions, including taste, swallowing, and salivation.
The motor fibers of the glossopharyngeal nerve innervate certain muscles involved in swallowing, such as the stylopharyngeus muscle. Additionally, these motor fibers play a role in controlling the gag reflex.
The glossopharyngeal nerve is a complex structure that extends throughout the head and neck region. It has numerous branches that innervate different areas and serve various functions. One of its branches, known as the tympanic nerve, provides sensory innervation to the middle ear. This allows us to perceive sounds and maintain proper hearing function.
Another important branch of the glossopharyngeal nerve is the carotid sinus nerve. This branch is responsible for carrying sensory information from the carotid sinus, a specialized area in the carotid artery that helps regulate blood pressure. Through this branch, the glossopharyngeal nerve contributes to the overall control of blood pressure and cardiovascular function.
Role and Function of the Glossopharyngeal Nerve
The glossopharyngeal nerve plays a vital role in many important bodily functions. It carries sensory information related to taste, touch, and temperature from the posterior third of the tongue. This information then reaches the brain, allowing us to experience the sensation of taste.
Moreover, the glossopharyngeal nerve is involved in the coordination of the swallowing process. It carries sensory information from the oropharynx, tonsils, and other related structures to the brain, allowing for the appropriate initiation and control of swallowing movements.
Furthermore, the glossopharyngeal nerve contributes to salivation, playing a significant role in the production and regulation of saliva. It also participates in the regulation of blood pressure by providing sensory inputs from certain baroreceptors located within the carotid sinus.
In addition to its sensory functions, the glossopharyngeal nerve also has motor functions that are essential for proper swallowing. The motor fibers of the glossopharyngeal nerve innervate the stylopharyngeus muscle, which plays a crucial role in elevating the pharynx during swallowing. This coordinated movement ensures that food and liquids pass smoothly from the mouth to the esophagus, preventing choking or aspiration.
Furthermore, the glossopharyngeal nerve is involved in the regulation of the gag reflex. This protective reflex helps prevent foreign objects from entering the airway by triggering a reflexive contraction of the muscles in the back of the throat. The glossopharyngeal nerve provides the necessary motor innervation to these muscles, ensuring the proper functioning of the gag reflex.
Overall, the glossopharyngeal nerve is a complex and multifunctional cranial nerve that plays a crucial role in various sensory and motor processes. Its intricate anatomy and extensive innervation allow for the coordination of essential functions such as taste, swallowing, salivation, and blood pressure regulation.
Disorders Associated with the Glossopharyngeal Nerve
Glossopharyngeal Neuralgia
Glossopharyngeal neuralgia is a rare condition characterized by recurring episodes of sharp, severe, and electric shock-like pain in the throat, tongue, tonsils, and ear. The exact cause of this condition is not well understood, but it is believed to result from the compression or irritation of the glossopharyngeal nerve.
The pain episodes can be triggered by various factors, including swallowing, speaking, coughing, or any movement that puts pressure on the glossopharyngeal nerve. Glossopharyngeal neuralgia is often challenging to diagnose, as the symptoms can mimic other conditions, such as dental problems or ear infections. Therefore, it is essential to consult with a healthcare professional for an accurate diagnosis and appropriate management.
Glossopharyngeal neuralgia can significantly impact a person’s quality of life. The excruciating pain experienced during episodes can be debilitating, making it difficult to perform daily activities. Individuals with this condition may find it challenging to eat, speak, or even engage in social interactions due to the fear of triggering an episode. Seeking proper medical care and support is crucial in managing glossopharyngeal neuralgia and improving overall well-being.
Various treatment options are available for glossopharyngeal neuralgia, depending on the severity and frequency of the pain episodes. Medications such as anticonvulsants or tricyclic antidepressants may be prescribed to help alleviate the pain. In some cases, nerve blocks or surgical interventions, such as microvascular decompression or radiofrequency ablation, may be considered to provide long-term relief.
Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can occur due to trauma, surgical complications, infections, tumors, or certain medical conditions, such as multiple sclerosis. When the glossopharyngeal nerve is damaged, it can lead to various symptoms, including difficulty swallowing, changes in taste sensation, hoarseness, and decreased salivation.
Damage to the glossopharyngeal nerve can significantly impact a person’s ability to eat and speak properly. Swallowing difficulties, known as dysphagia, can lead to malnutrition and weight loss if not properly managed. Changes in taste sensation can affect a person’s enjoyment of food and may lead to a loss of appetite. Hoarseness and decreased salivation can also affect speech clarity and overall oral health.
The treatment options for glossopharyngeal nerve damage depend on the underlying cause and severity of the damage. It is crucial to consult with a healthcare professional to determine the appropriate course of action. Physical therapy and swallowing exercises may be recommended to improve swallowing function. In some cases, surgical interventions or nerve regeneration techniques may be considered to restore nerve function and alleviate symptoms.
Living with glossopharyngeal nerve damage can be challenging, but with proper medical care and support, individuals can learn to manage their symptoms and improve their quality of life. Speech and swallowing therapy, along with dietary modifications, can help individuals regain their ability to eat and communicate effectively.
Tumors Affecting the Glossopharyngeal Nerve
Tumors can also affect the glossopharyngeal nerve, causing compression and potentially leading to various symptoms. These tumors can be benign (non-cancerous) or malignant (cancerous), and their treatment options depend on their nature and location. Typically, surgical intervention and, in some cases, radiation therapy or chemotherapy may be considered.
The presence of tumors near the glossopharyngeal nerve can cause a range of symptoms, depending on their size and location. Common symptoms include pain, difficulty swallowing, changes in voice, and facial weakness. These symptoms can significantly impact a person’s daily life, making it challenging to eat, speak, or perform routine activities.
When tumors affecting the glossopharyngeal nerve are detected, a multidisciplinary approach involving various healthcare professionals, such as neurosurgeons, oncologists, and radiation therapists, is often necessary. The treatment plan will depend on factors such as the tumor’s size, location, and whether it is benign or malignant. Surgery may be performed to remove the tumor, and radiation therapy or chemotherapy may be recommended to target any remaining cancer cells.
Living with a tumor affecting the glossopharyngeal nerve can be emotionally and physically challenging. Support from healthcare professionals, as well as family and friends, is crucial in navigating the treatment process and managing the associated symptoms. Rehabilitation services, including speech therapy and physical therapy, may be beneficial in helping individuals regain function and improve their overall well-being.
Symptoms and Diagnosis of Glossopharyngeal Nerve Disorders
Common Symptoms
Glossopharyngeal nerve disorders can present with a range of symptoms, including throat pain, difficulty swallowing, changes in taste sensation, ear pain, hoarseness, voice changes, and decreased salivation. Each individual may experience a unique combination of symptoms, and the severity can vary.
Throat pain is a common symptom experienced by individuals with glossopharyngeal nerve disorders. This pain can range from a mild discomfort to a sharp, stabbing sensation. It may be localized to a specific area or radiate to other parts of the throat. The pain can be aggravated by swallowing, talking, or even just moving the neck.
Difficulty swallowing, also known as dysphagia, is another common symptom of glossopharyngeal nerve disorders. Individuals may have trouble swallowing both solids and liquids, and this can lead to weight loss and malnutrition if not properly managed. The sensation of food getting stuck in the throat or the feeling of choking while eating or drinking are also frequently reported.
Changes in taste sensation can be quite distressing for individuals with glossopharyngeal nerve disorders. They may experience a metallic or bitter taste in their mouth, or they may find that certain foods no longer taste the way they used to. This can greatly affect their enjoyment of meals and overall quality of life.
Ear pain is another symptom that can be associated with glossopharyngeal nerve disorders. This pain may be felt deep within the ear or radiate from the throat. It can be sharp, throbbing, or a constant dull ache. Some individuals may also experience ringing in the ears, known as tinnitus.
Hoarseness and voice changes are common symptoms of glossopharyngeal nerve disorders. The voice may become weak, raspy, or strained. Individuals may have difficulty projecting their voice or speaking for extended periods of time without experiencing fatigue.
Decreased salivation, also known as dry mouth or xerostomia, is another symptom that individuals with glossopharyngeal nerve disorders may experience. This can lead to difficulties with chewing and swallowing, as well as an increased risk of dental problems such as tooth decay and gum disease.
Diagnostic Procedures
Diagnosing glossopharyngeal nerve disorders often involves a comprehensive evaluation of the individual’s medical history, physical examination, and possibly additional tests. These tests may include imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, electromyography (EMG), nerve conduction studies, and possibly blood tests.
Magnetic resonance imaging (MRI) and computed tomography (CT) scans are commonly used to visualize the structures in the throat and neck. These imaging studies can help identify any abnormalities or lesions that may be affecting the glossopharyngeal nerve.
Electromyography (EMG) is a diagnostic test that measures the electrical activity of muscles. In the case of glossopharyngeal nerve disorders, EMG can help determine if there is any dysfunction or damage to the muscles involved in swallowing and speaking.
Nerve conduction studies are another diagnostic tool that can be used to assess the function of the glossopharyngeal nerve. These studies involve applying small electrical currents to specific areas of the body and measuring the speed and strength of the nerve signals. Abnormal results can indicate nerve damage or dysfunction.
Blood tests may also be ordered to rule out any underlying medical conditions that could be contributing to the glossopharyngeal nerve disorder. These tests can help identify potential causes such as infections, autoimmune disorders, or vitamin deficiencies.
Due to the complex nature of these disorders and the potential for various underlying causes, it is crucial to consult with a healthcare professional who specializes in neurology or otolaryngology to ensure an accurate diagnosis and appropriate management plan. They will be able to interpret the results of the diagnostic tests and recommend the most effective treatment options for each individual case.
Treatment Options for Glossopharyngeal Nerve Disorders
Glossopharyngeal nerve disorders can significantly impact an individual’s daily life, causing discomfort and pain. Fortunately, there are various treatment options available to alleviate symptoms, manage underlying causes, and improve the individual’s quality of life.
Medication and Non-Surgical Treatments
One of the primary approaches to treating glossopharyngeal nerve disorders is through medication. Healthcare professionals may prescribe anticonvulsants or tricyclic antidepressants to help control pain or reduce nerve irritation. These medications work by modulating the activity of the nerves, providing relief and improving the individual’s overall well-being.
In addition to medication, non-surgical treatments can also be considered. Nerve blocks, which involve injecting an anesthetic or steroid around the affected nerve, can provide temporary relief from pain and discomfort. Another non-surgical option is radiofrequency ablation, a procedure that uses heat to destroy the problematic nerve fibers, offering long-lasting symptom management.
It is important to note that these non-surgical treatments should only be performed by qualified healthcare professionals who have extensive experience in these procedures. Their expertise ensures the safety and effectiveness of the interventions.
Surgical Interventions
In certain cases, surgical intervention may be necessary to address the underlying cause of the glossopharyngeal nerve disorder or provide long-term symptom relief. The decision to undergo surgery is typically made after careful consideration of the individual’s condition and consultation with healthcare professionals who specialize in neurosurgery or otolaryngology.
One surgical option is nerve decompression, which involves relieving pressure on the glossopharyngeal nerve by removing nearby structures or tissues that may be compressing it. This procedure aims to restore normal nerve function and alleviate symptoms.
Another surgical approach is neurectomy, which involves the surgical removal of part of the glossopharyngeal nerve. This procedure is typically reserved for severe cases where other treatment options have been ineffective. Neurectomy aims to permanently eliminate the source of pain and discomfort, providing long-term relief.
In rare instances where a tumor is causing the glossopharyngeal nerve disorder, surgical tumor removal may be necessary. This procedure involves removing the tumor, relieving pressure on the nerve, and addressing the underlying cause of the disorder.
It is crucial to consult with a healthcare professional who specializes in neurosurgery or otolaryngology to determine the best course of action based on individual circumstances. They will carefully evaluate the individual’s condition, consider all available treatment options, and recommend the most suitable approach for optimal outcomes.
Prevention and Management of Glossopharyngeal Nerve Disorders
Lifestyle Modifications
Some lifestyle modifications might help manage glossopharyngeal nerve disorders and reduce the frequency or severity of symptoms. These modifications can include avoiding trigger factors such as certain foods, maintaining good oral hygiene, practicing stress management techniques, and engaging in gentle throat exercises, as advised by a healthcare professional.
Moreover, maintaining a healthy lifestyle, including a balanced diet, regular exercise, and adequate rest, can contribute to overall well-being and potentially support the body in managing any underlying conditions associated with glossopharyngeal nerve disorders.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation programs may be beneficial for individuals experiencing functional limitations due to glossopharyngeal nerve disorders. These programs can help improve swallowing coordination, enhance vocal quality, and provide strategies to manage symptoms effectively. It is essential to consult with a healthcare professional to determine the appropriateness and potential benefits of physical therapy and rehabilitation in individual cases.
Future Research Directions in Glossopharyngeal Nerve Disorders
Emerging Therapies
Research and development in the field of glossopharyngeal nerve disorders continue to advance, leading to the emergence of innovative therapies. These therapies may include novel medications, minimally invasive procedures, or neuromodulation techniques aimed at providing enhanced symptom relief and improved quality of life for affected individuals.
It is important to note that these emerging therapies are still being investigated and may not be widely available. Their safety and effectiveness need to be thoroughly evaluated through clinical trials and approved by appropriate regulatory authorities before becoming standard treatment options.
Advances in Diagnostic Techniques
The development of advanced diagnostic techniques and technologies plays an integral role in improving the accuracy and efficiency of diagnosing glossopharyngeal nerve disorders. Continual research efforts aim to refine existing imaging modalities, develop new biomarkers, and enhance our understanding of the complex mechanisms underlying these disorders.
Advances in diagnostic techniques have the potential to facilitate earlier detection, facilitate personalized treatment planning, and improve overall patient outcomes. However, it is essential to consult with a healthcare professional who can utilize these advancements appropriately and interpret the results accurately.
In conclusion, understanding the function and disorders of the glossopharyngeal nerve is paramount to grasp the intricate nature of this crucial nerve’s role in various bodily functions. Recognizing the symptoms, seeking a comprehensive diagnosis, and exploring appropriate treatment options with the guidance of healthcare professionals can help individuals affected by glossopharyngeal nerve disorders effectively manage their condition and improve their quality of life.