The glossopharyngeal nerve is a crucial component of the human nervous system. As medical professionals, nurses play an integral role in assessing the functionality of this important nerve. One way they evaluate the glossopharyngeal nerve is by testing specific reflexes associated with it. By understanding the anatomy, functions, and potential disorders of the glossopharyngeal nerve, nurses can provide accurate and comprehensive assessments to their patients.
Understanding the Glossopharyngeal Nerve
Anatomy of the Glossopharyngeal Nerve
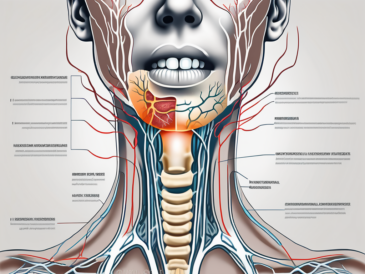
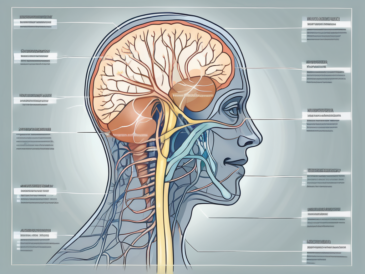
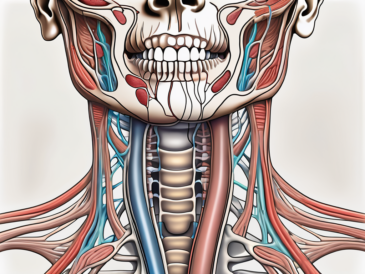
The glossopharyngeal nerve, also known as cranial nerve IX, arises from the medulla oblongata. It primarily innervates the back third of the tongue, the tonsils, the soft palate, and certain muscles of the throat. This nerve also carries sensory information from the carotid sinus and carotid body, which are vital in monitoring blood pressure and oxygen levels, respectively.
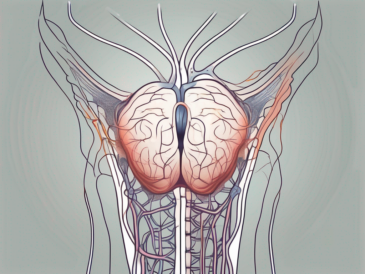
The medulla oblongata, located at the base of the brainstem, is a crucial structure involved in the regulation of various bodily functions. It serves as a relay station for sensory and motor signals traveling between the brain and the spinal cord. The glossopharyngeal nerve emerges from the medulla oblongata, branching out to supply innervation to specific regions of the oral cavity and throat.
The back third of the tongue, known as the posterior third, is responsible for detecting taste sensations. The glossopharyngeal nerve plays a significant role in transmitting gustatory information from this region to the brain. This allows us to savor the flavors of different foods and beverages, enhancing our overall sensory experience.
In addition to its role in taste sensation, the glossopharyngeal nerve is also involved in the coordination of swallowing actions. When we swallow, a complex series of muscular contractions occurs in the throat, allowing food and liquids to pass from the mouth into the esophagus. The glossopharyngeal nerve helps to orchestrate this process, ensuring that the muscles of the pharynx work together seamlessly.
Furthermore, the glossopharyngeal nerve contributes to the gag reflex, a protective mechanism that helps prevent choking. When an object or substance stimulates the back of the throat, the glossopharyngeal nerve sends signals to trigger a reflexive contraction of the throat muscles. This reflexive action helps expel the foreign object or substance, safeguarding the airway and preventing potential harm.
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve performs various crucial functions. It plays a significant role in taste sensation, transmitting gustatory information from the posterior third of the tongue. Additionally, this nerve is involved in the swallowing reflex, allowing the muscles of the pharynx to coordinate swallowing actions effectively. Moreover, the glossopharyngeal nerve contributes to the gag reflex, a protective mechanism vital for preventing choking.
Aside from its involvement in taste, swallowing, and the gag reflex, the glossopharyngeal nerve also carries sensory information from the carotid sinus and carotid body. The carotid sinus is a small, dilated area located at the beginning of the internal carotid artery, one of the major blood vessels supplying the brain. It contains specialized cells that detect changes in blood pressure. When blood pressure increases, the glossopharyngeal nerve relays this information to the brain, triggering appropriate adjustments to maintain cardiovascular homeostasis.
The carotid body, on the other hand, is a small cluster of chemoreceptor cells located near the carotid bifurcation. These cells are responsible for monitoring the levels of oxygen and carbon dioxide in the blood. When oxygen levels drop or carbon dioxide levels rise, the glossopharyngeal nerve transmits signals to the brain, prompting adjustments in breathing rate and depth to ensure adequate oxygenation.
Overall, the glossopharyngeal nerve is a multifunctional cranial nerve that plays a crucial role in various sensory and motor processes. Its intricate connections and contributions to taste, swallowing, the gag reflex, and the monitoring of blood pressure and oxygen levels highlight its significance in maintaining overall health and well-being.
The Role of Nurses in Neurological Assessments
Importance of Neurological Assessments
Neurological assessments are integral in evaluating the overall functioning of the nervous system. These evaluations help identify potential neurological disorders, monitor disease progression, and guide treatment plans. Nurses, trained to administer neurological assessments, play a fundamental role in early detection, intervention, and patient care.
When it comes to neurological assessments, nurses are at the forefront of patient care. They are responsible for conducting thorough assessments to gather vital information about the patient’s neurological status. By carefully observing and documenting the patient’s responses, nurses can detect any abnormalities or changes that may indicate a neurological disorder.
Furthermore, nurses play a crucial role in educating patients and their families about the importance of neurological assessments. They explain the significance of these assessments in monitoring the progression of neurological conditions and adjusting treatment plans accordingly. By providing this education, nurses empower patients to actively participate in their own care and make informed decisions about their health.
Skills Required for Neurological Assessments
Performing neurological assessments requires a range of skills that nurses acquire through training and experience. These skills encompass an understanding of anatomical structures, proficiency in conducting reflex tests, and the ability to communicate effectively with patients. Nurses must also possess critical thinking skills to accurately interpret assessment results and identify potential abnormalities.
When it comes to understanding anatomical structures, nurses must have a comprehensive knowledge of the nervous system. This includes understanding the different parts of the brain, spinal cord, and peripheral nerves. By having this knowledge, nurses can accurately assess and interpret any abnormalities they may encounter during the assessment process.
In addition to anatomical knowledge, nurses must also be proficient in conducting reflex tests. These tests involve assessing the patient’s reflexes, such as the knee-jerk reflex or the pupillary reflex. By performing these tests, nurses can evaluate the integrity of the patient’s nervous system and identify any potential issues.
Effective communication is another essential skill for nurses conducting neurological assessments. They must be able to establish a rapport with their patients, making them feel comfortable and at ease during the assessment. By creating a trusting relationship, nurses can gather more accurate information and ensure that the patient feels heard and understood.
Lastly, critical thinking skills are vital for nurses when interpreting assessment results. They must be able to analyze the gathered data, compare it to normal values, and identify any deviations or abnormalities. This requires nurses to have a deep understanding of neurological conditions and their associated signs and symptoms.
In conclusion, nurses play a crucial role in neurological assessments. Their skills, knowledge, and expertise are essential in early detection, intervention, and patient care. By conducting thorough assessments and interpreting the results accurately, nurses contribute significantly to the overall well-being of patients with neurological disorders.
Reflexes Associated with the Glossopharyngeal Nerve
The Gag Reflex and its Significance
The gag reflex, mediated by the glossopharyngeal nerve, is a protective mechanism that prevents foreign objects from entering the airway during swallowing. When the back of the throat is stimulated, this reflex triggers a contraction of the throat muscles, eliciting the urge to gag. The absence or abnormality of the gag reflex may indicate underlying neurological issues and should be further investigated.
The gag reflex is a fascinating physiological response that plays a crucial role in safeguarding our respiratory system. It is an involuntary reaction that occurs when the soft palate, back of the tongue, or throat is touched, triggering a complex chain of events. The glossopharyngeal nerve, also known as the ninth cranial nerve, is responsible for transmitting the sensory information from these areas to the brainstem.
Upon stimulation, the glossopharyngeal nerve sends signals to the medulla oblongata, the lower part of the brainstem. Here, the information is processed, and a motor response is generated. The medulla oblongata coordinates the contraction of various muscles involved in the gag reflex, including the muscles of the pharynx, larynx, and diaphragm.
Interestingly, the gag reflex is not only a protective mechanism but also serves as an essential diagnostic tool. Healthcare professionals, such as doctors and dentists, often test the gag reflex to assess the integrity of the glossopharyngeal nerve and other associated cranial nerves. The absence or abnormality of the gag reflex can indicate nerve damage or dysfunction, which may be caused by conditions like stroke, tumors, or infections.
Swallowing Reflex and its Role
In collaboration with other cranial nerves, the glossopharyngeal nerve coordinates the complex process of swallowing. This reflex involves a series of precisely timed muscle contractions, allowing food and liquids to pass from the mouth to the stomach. Nurses must evaluate the swallowing reflex to identify any impairment that could lead to nutritional deficiencies or aspiration.
Swallowing is a remarkable physiological process that we often take for granted. It involves the coordinated effort of multiple muscles and nerves, working seamlessly to transport food and liquids from the oral cavity to the esophagus. The glossopharyngeal nerve plays a vital role in this intricate process, ensuring the smooth passage of ingested substances.
When we consume food or drink, the tongue initiates the swallowing reflex by pushing the bolus (chewed food) towards the back of the throat. As the bolus reaches the oropharynx, sensory receptors in the area detect its presence and send signals to the brainstem via the glossopharyngeal nerve.
The brainstem then orchestrates a series of muscle contractions, known as peristalsis, that propel the bolus through the pharynx and into the esophagus. This coordinated movement involves the contraction and relaxation of various muscles, including those innervated by the glossopharyngeal nerve.
It is crucial for healthcare professionals, particularly nurses, to assess the swallowing reflex in patients. Impairments in swallowing, known as dysphagia, can lead to serious complications such as malnutrition, dehydration, and aspiration pneumonia. By evaluating the function of the glossopharyngeal nerve and other cranial nerves involved in swallowing, nurses can identify any abnormalities and implement appropriate interventions to ensure safe and efficient swallowing.
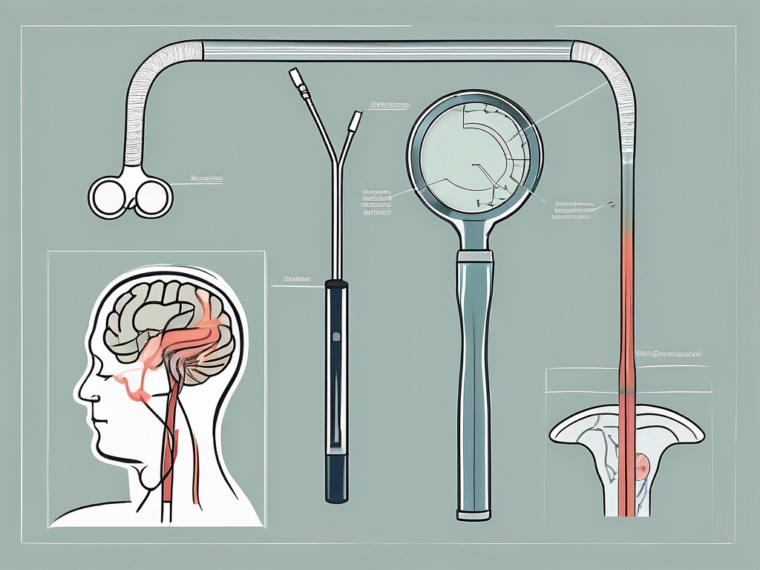
Procedure for Testing Glossopharyngeal Nerve Reflexes
Preparing the Patient for the Test
Prior to conducting the reflex tests, nurses must ensure the patient is comfortable and appropriately positioned. This includes providing a calm and quiet environment to minimize any potential distractions or discomfort. Clear instructions should be provided, explaining the purpose of the test and what the patient can expect to experience. It is important for the nurse to address any potential concerns or risks that the patient may have, ensuring that they feel informed and at ease.
Obtaining informed consent is an essential part of the preparation process. The nurse should explain the procedure in detail, including the specific reflexes that will be tested and the sensations that the patient may feel during the test. This allows the patient to make an informed decision about their participation and ensures that they are fully aware of what to expect.
Steps in Performing the Gag Reflex Test
Conducting the gag reflex test involves gently stimulating the back of the throat with a tongue depressor or a cotton swab. The nurse carefully places the instrument at the back of the patient’s tongue, applying slight pressure to trigger the reflex. It is important for the nurse to be gentle and cautious during this process, as excessive force or discomfort can lead to an inaccurate response.
As the nurse stimulates the back of the throat, they observe the patient’s response closely. The gag reflex is a protective mechanism that prevents foreign objects from entering the airway, so a normal response would involve the patient coughing, gagging, or feeling the need to swallow. The nurse assesses the adequacy and symmetry of the reflex, noting any variations or abnormalities in the patient’s response.
Throughout the test, the nurse communicates with the patient, providing reassurance and support. They may ask the patient to indicate any discomfort or unusual sensations they experience during the test. This open line of communication allows the nurse to gather valuable information and ensures the patient’s comfort and well-being throughout the procedure.
Interpreting the Results of the Reflex Test
After performing the reflex tests, nurses must interpret the results in the context of the patient’s overall health and medical history. The presence of a normal gag reflex and appropriate swallowing reflex suggests proper glossopharyngeal nerve function. These reflexes indicate that the nerves responsible for these functions are intact and functioning correctly.
However, abnormalities in these reflexes may indicate nerve damage, disorders, or other underlying medical conditions that necessitate further investigation by a healthcare professional. If the patient exhibits an exaggerated or absent gag reflex, it could be a sign of glossopharyngeal nerve dysfunction. This could be caused by various factors such as trauma, infection, inflammation, or neurological conditions.
It is crucial for the nurse to document any abnormal findings or variations from the expected response. This documentation provides a comprehensive record of the patient’s reflexes and can assist in the diagnosis and treatment of any underlying issues. The nurse should include details such as the patient’s reaction, the strength and symmetry of the reflex, and any other relevant observations.
In conclusion, testing glossopharyngeal nerve reflexes is an important component of a comprehensive neurological assessment. By following the proper procedure and paying attention to the patient’s responses, nurses can gather valuable information about the functioning of the glossopharyngeal nerve. This information can aid in the diagnosis and treatment of various medical conditions, ensuring the best possible care for the patient.
Potential Abnormalities and Disorders of the Glossopharyngeal Nerve
Symptoms Indicating Glossopharyngeal Nerve Damage
In some cases, damage or dysfunction in the glossopharyngeal nerve can give rise to specific symptoms. These may include impaired taste sensation, difficulty swallowing, referred pain in the throat or ear, excessive drooling, and voice changes. Patients experiencing these symptoms should promptly consult with a healthcare provider for a comprehensive evaluation and appropriate management.
Conditions Affecting the Glossopharyngeal Nerve
Several medical conditions can affect the glossopharyngeal nerve. Neuralgia, an intense facial pain condition, can radiate along the distribution of the glossopharyngeal nerve, causing significant discomfort. Tumors, infections, and inflammation can also affect the functionality of this nerve, leading to various symptoms. Accurate diagnosis and treatment of these conditions require the expertise of a healthcare professional.
The Role of Reflex Testing in Diagnosing Glossopharyngeal Nerve Disorders
Importance of Reflex Testing in Diagnosis
Reflex testing serves as an invaluable diagnostic tool in assessing the integrity of the glossopharyngeal nerve and identifying potential disorders. Abnormal reflex responses provide valuable clues to guide further investigations, aiding healthcare professionals in formulating accurate diagnoses and designing appropriate treatment plans. It is essential to understand that reflex testing is only one aspect of a comprehensive neurological assessment.
Limitations of Reflex Testing
While reflex testing can provide valuable insights, it does have some limitations. Abnormal reflexes can result from factors other than glossopharyngeal nerve dysfunction, such as anxiety or medication side effects. Additionally, reflex testing alone cannot provide a definitive diagnosis. Thus, it is crucial for patients with concerning symptoms to consult with a healthcare professional for a comprehensive evaluation and proper diagnostic approach.
Safety Measures and Considerations during Reflex Testing
Ensuring Patient Comfort and Safety
During reflex testing, nurses should prioritize the comfort and safety of their patients. Adequate explanation of the procedure, attentive listening to patient concerns, and a supportive environment can help alleviate anxiety. Careful adherence to infection control measures and use of sterile equipment is essential to prevent potential complications. Every precaution should be taken to minimize any discomfort or risk associated with the reflex testing process.
Dealing with Abnormal Reflex Responses
If a patient demonstrates abnormal reflex responses, nurses should promptly report these findings to the appropriate healthcare professionals. Accurate documentation of abnormal reflexes, including the nature of the response and any accompanying symptoms, is crucial for effective communication and collaborative patient care. By working together with other healthcare team members, nurses can contribute to the timely identification and management of glossopharyngeal nerve disorders.
In conclusion, the glossopharyngeal nerve plays a vital role in several essential functions of the human body, including taste sensation, swallowing, and the gag reflex. Nurses, equipped with the necessary skills and knowledge, are pivotal in assessing the functionality of this nerve through reflex testing. While reflex testing aids in identifying potential neurological disorders, it should always be complemented by a comprehensive evaluation conducted by healthcare professionals. By adhering to safety measures, exhibiting expertise, and prioritizing patient comfort, nurses can contribute to the accurate assessment and management of glossopharyngeal nerve-related conditions. If you have any questions or concerns regarding your symptoms or health, it is always recommended to consult with a healthcare provider for appropriate guidance and care.