The glossopharyngeal nerve is a crucial component of our nervous system, responsible for providing sensory information and controlling vital functions in the head and throat region. Damage to this nerve can result in various complications and debilitating symptoms that can significantly impact an individual’s quality of life. Understanding glossopharyngeal nerve damage is essential for clinicians and patients alike, as it helps in early detection, diagnosis, and appropriate treatment strategies.
Understanding the Glossopharyngeal Nerve
Anatomy of the Glossopharyngeal Nerve
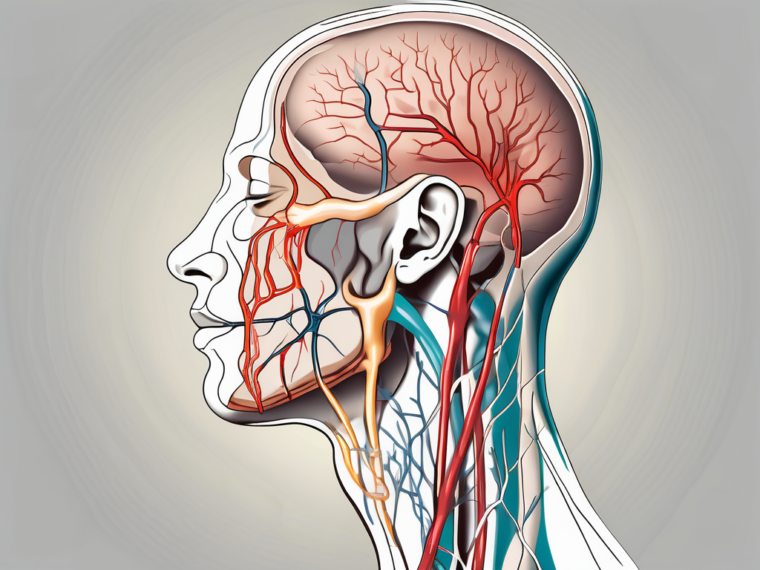
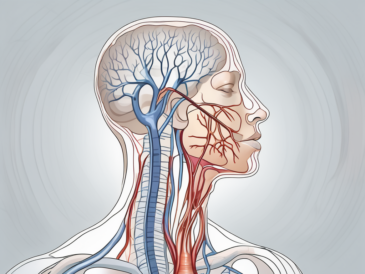
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves that emerge directly from the brain. It consists of both sensory and motor fibers, originating from the medulla oblongata at the base of the brain. From there, it extends downwards, passing through various structures in the head and neck region.
The glossopharyngeal nerve innervates specific areas, including the back of the throat (oropharynx), tongue, tonsils, and middle ear. Its branches also provide sensation to the eardrum, the carotid body (a structure that helps regulate blood pressure), and certain regions of the brain.
As the glossopharyngeal nerve travels through the head and neck, it forms connections with other cranial nerves, such as the vagus nerve and the accessory nerve. These connections allow for coordinated movements and sensory perception in the region.
The glossopharyngeal nerve is a complex structure, with multiple branches that serve different functions. One of its branches, the tympanic nerve, carries sensory information from the middle ear to the brain. This allows us to perceive sound and maintain balance.
Function of the Glossopharyngeal Nerve
The glossopharyngeal nerve plays a vital role in essential functions such as taste sensation, swallowing, salivation, and monitoring blood pressure. It carries sensory information from the tongue, tonsils, and throat to the brain, allowing us to perceive taste and touch in these areas. Additionally, it provides motor function to the stylopharyngeus muscle, which helps in swallowing and speech production.
In addition to its sensory and motor functions, the glossopharyngeal nerve also has autonomic functions. It is involved in regulating blood pressure through its connections with the carotid body, a small structure located in the carotid artery. The carotid body senses changes in blood oxygen levels and sends signals to the brain via the glossopharyngeal nerve, which then triggers appropriate adjustments in blood pressure.
Furthermore, the glossopharyngeal nerve is responsible for initiating the gag reflex, a protective mechanism that helps prevent choking. When stimulated, the nerve sends signals to the brain, which in turn triggers a series of coordinated muscle contractions in the throat and esophagus to expel any potential obstructions.
Overall, the glossopharyngeal nerve is a crucial component of the nervous system, playing a significant role in various sensory, motor, and autonomic functions. Its intricate connections and widespread innervation make it an essential part of our ability to taste, swallow, speak, and regulate blood pressure.
Causes of Glossopharyngeal Nerve Damage
The glossopharyngeal nerve is a crucial component of the nervous system responsible for various functions in the head and neck region. Damage to this nerve can occur due to several factors, including trauma and injury, medical conditions and diseases, as well as surgical complications.
Trauma and Injury
Traumatic events such as accidents or sports-related injuries can damage the glossopharyngeal nerve. Direct trauma to the head or neck region, fractures of the skull or jaw, or penetrating injuries can inadvertently affect the nerve’s integrity.
For instance, a severe blow to the head during a car accident can result in the compression or stretching of the glossopharyngeal nerve, leading to potential damage. Similarly, a sports-related injury involving a forceful impact to the neck can also impact the nerve’s function.
It is crucial to seek immediate medical attention if a head or neck injury occurs, as prompt evaluation by healthcare professionals can aid in the early detection of glossopharyngeal nerve damage. Early intervention and appropriate treatment can help minimize long-term complications and improve outcomes.
Medical Conditions and Diseases
Various medical conditions and diseases can also lead to glossopharyngeal nerve damage. Examples include certain types of tumors, infections, and inflammatory disorders affecting the head and neck region, such as glossopharyngeal neuralgia or glossopharyngeal schwannoma.
Glossopharyngeal neuralgia is a condition characterized by severe, recurring pain in the throat, tongue, ear, or tonsils. This pain can be triggered by activities such as swallowing, speaking, or even touching the affected area. In some cases, the underlying cause of glossopharyngeal neuralgia may be the presence of a tumor or other structural abnormalities affecting the nerve.
If you are experiencing persistent symptoms, such as difficulty swallowing, sudden-onset pain in the throat or ear, or unexplained changes in blood pressure, it is vital to consult with a healthcare professional for a thorough assessment and appropriate management. Identifying the underlying medical condition causing the glossopharyngeal nerve damage is crucial for developing an effective treatment plan.
Surgical Complications
In some cases, surgical interventions in the head and neck region may inadvertently damage the glossopharyngeal nerve. Surgeons take precautions to minimize injury, but complications can still arise. Such complications can occur during surgeries for tumors, glandular disorders, or other surgical procedures involving the throat or middle ear.
During surgical procedures, the glossopharyngeal nerve may be at risk of injury due to its proximity to the surgical site. Surgeons must exercise caution and employ meticulous techniques to minimize the risk of nerve damage. However, despite these precautions, unforeseen circumstances or anatomical variations can make the nerve vulnerable to injury.
If you are scheduled for surgery or have undergone a procedure in the head and neck area and notice persistent symptoms affecting taste, swallowing, or blood pressure, it is essential to report them to your healthcare provider promptly. Early detection and appropriate management of surgical complications can help prevent further damage and promote optimal recovery.
In conclusion, glossopharyngeal nerve damage can occur due to various causes, including trauma and injury, medical conditions and diseases, as well as surgical complications. Understanding the potential risk factors and seeking timely medical attention can play a crucial role in the diagnosis, treatment, and management of glossopharyngeal nerve damage.
Symptoms of Glossopharyngeal Nerve Damage
Physical Symptoms
Glossopharyngeal nerve damage can manifest in various ways, including physical symptoms. These symptoms may include difficulty swallowing (dysphagia), changes in taste perception, persistent throat or ear pain, or weakness in the muscles involved in speech production.
If you notice any of these symptoms persistently, it is crucial to consult with a healthcare professional for a proper evaluation. A thorough physical examination and additional diagnostic tests may be necessary to identify the root cause and develop an appropriate treatment plan tailored to your specific needs.
Difficulty swallowing, also known as dysphagia, can be a distressing symptom that affects the overall quality of life. It can lead to the avoidance of certain foods and beverages, resulting in nutritional deficiencies. In severe cases, dysphagia can even lead to aspiration pneumonia, a potentially life-threatening condition where food or liquid enters the lungs instead of the stomach.
Changes in taste perception can be frustrating and may impact one’s enjoyment of food. Imagine biting into your favorite dish, only to find that it tastes completely different or even unpleasant. This alteration in taste sensation can be caused by the glossopharyngeal nerve’s impairment, affecting the taste buds located at the back of the tongue and throat.
Individuals with glossopharyngeal nerve damage may experience persistent throat or ear pain. This discomfort can range from mild to severe and may be accompanied by a sensation of pressure or fullness. The pain can make it challenging to eat, speak, or even concentrate on daily tasks.
Weakness in the muscles involved in speech production, such as the tongue and throat muscles, can make it difficult to articulate words clearly. This can lead to speech difficulties, affecting communication and social interactions.
Sensory Symptoms
Impairment of the glossopharyngeal nerve can result in sensory symptoms, such as altered taste perception or a lack of taste sensation in the back of the tongue or throat. Some individuals may experience a persistent metallic or bitter taste. These sensory disturbances can significantly impact one’s ability to enjoy food and beverages.
If you encounter persistent changes in taste perception or other sensory disturbances, it is advisable to seek medical advice. A healthcare professional can evaluate your symptoms and provide guidance on appropriate management approaches.
Altered taste perception can lead to a diminished appetite and reduced food intake. This can result in weight loss and malnutrition if not addressed promptly. Additionally, the persistent metallic or bitter taste can make it challenging to consume certain foods, leading to a limited diet and potential nutrient deficiencies.
The lack of taste sensation in the back of the tongue or throat can also affect the enjoyment of eating. Taste plays a crucial role in our overall sensory experience of food, and when it is compromised, meals may become less pleasurable and satisfying.
Impact on Daily Life
The symptoms associated with glossopharyngeal nerve damage can significantly impact an individual’s daily life. Difficulties with swallowing can affect nutrition and hydration, potentially leading to weight loss or dehydration. Taste changes can diminish the pleasure derived from eating and may even affect appetite.
It is crucial to seek medical advice if your symptoms are interfering with your daily life. Your healthcare provider can suggest appropriate interventions, such as dietary modifications or speech therapy, to alleviate the impact on your overall well-being.
In addition to the physical and sensory symptoms, glossopharyngeal nerve damage can also have psychological and emotional effects. The frustration and distress caused by difficulties in swallowing or changes in taste perception can lead to anxiety, depression, or social isolation. It is essential to address these emotional aspects of living with glossopharyngeal nerve damage through counseling or support groups.
Furthermore, the impact on daily life extends beyond eating and drinking. Speech difficulties resulting from weakness in the muscles involved in speech production can affect professional and personal interactions. It may be challenging to communicate effectively, leading to misunderstandings or difficulties in expressing oneself.
Living with glossopharyngeal nerve damage requires a multidisciplinary approach to address the various aspects of its impact. Collaborating with healthcare professionals, including neurologists, speech therapists, nutritionists, and mental health specialists, can help individuals develop coping strategies and regain a sense of control over their lives.
Diagnosis of Glossopharyngeal Nerve Damage
Medical History and Physical Examination
Diagnosing glossopharyngeal nerve damage often involves a comprehensive medical history assessment and a thorough physical examination. Your healthcare provider will inquire about your symptoms, their duration and severity, and any factors that exacerbate or alleviate them. A detailed exploration of your medical history can help identify potential underlying causes or contributing factors.
During the physical examination, your healthcare provider may assess your throat, tongue, and sensation in the affected areas. They may also evaluate your ability to swallow and perform certain speech-related tasks. These evaluations help in pinpointing the nerve damage and formulating an accurate diagnosis.
For example, during the physical examination, your healthcare provider may use a tongue depressor to examine your throat and tongue. They may also use a cotton swab to test the sensation in the affected areas. By observing your ability to swallow and perform speech-related tasks, they can assess the functionality of the glossopharyngeal nerve.
Furthermore, your healthcare provider may ask you to describe any pain or discomfort you experience in the affected areas. This information can provide valuable insights into the nature and intensity of the nerve damage.
Imaging and Laboratory Tests
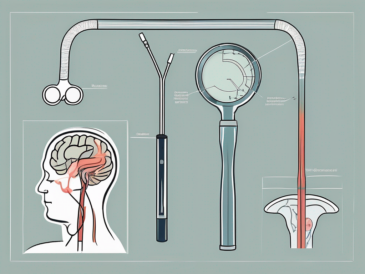
In some cases, additional diagnostic tests may be necessary to confirm glossopharyngeal nerve damage and identify underlying causes. Imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans can provide detailed views of the head and neck region to identify structural abnormalities or tumors affecting the nerve.
During an MRI or CT scan, you will lie on a table that slides into a large, tunnel-like machine. The machine uses powerful magnets and radio waves to create detailed images of the inside of your body. These images can help your healthcare provider visualize any abnormalities or damage to the glossopharyngeal nerve.
Laboratory tests, including blood work, may be ordered to rule out systemic causes or detect any changes in blood parameters that may suggest an underlying medical condition contributing to the nerve damage. Blood tests can help identify any infections, inflammation, or metabolic disorders that may be affecting the nerve.
For example, your healthcare provider may order a complete blood count (CBC) to check for any signs of infection or inflammation. They may also request specific blood tests to assess your thyroid function or blood sugar levels, as these can sometimes contribute to nerve damage.
Differential Diagnosis
Diagnosing glossopharyngeal nerve damage requires considering other potential causes of similar symptoms. Some conditions that can present similarly include other cranial nerve disorders, temporomandibular joint dysfunction, or gastrointestinal disorders. A comprehensive evaluation of the symptoms, medical history, and results of additional tests aids in accurately distinguishing glossopharyngeal nerve damage from other conditions.
During the differential diagnosis process, your healthcare provider will carefully analyze your symptoms and compare them to the characteristic features of various conditions. They may also consult with other specialists, such as neurologists or otolaryngologists, to ensure an accurate diagnosis.
It is important to consult with a healthcare professional to receive a proper diagnosis. They can guide you through the diagnostic process and recommend the most appropriate course of action based on your individual circumstances.
Remember, early diagnosis and intervention can significantly improve the prognosis and quality of life for individuals with glossopharyngeal nerve damage.
Treatment Options for Glossopharyngeal Nerve Damage
Medications and Therapies
The management of glossopharyngeal nerve damage depends on the underlying cause, severity of symptoms, and individual patient factors. Medications may be prescribed to alleviate pain, control blood pressure, or manage associated conditions such as acid reflux, which can worsen symptoms.
Physical therapy and swallowing exercises may be recommended to improve muscle strength and enhance swallowing function. Speech therapy can assist in addressing speech-related difficulties, such as articulation or voice changes.
Surgical Interventions
In some cases, surgical interventions may be required to treat glossopharyngeal nerve damage. The decision to proceed with surgery depends on factors such as the underlying cause, severity of symptoms, and overall health of the patient.
Surgical options may include nerve repair procedures, removal of tumors, or interventions to relieve pressure on the nerve. Your healthcare provider will discuss the potential benefits, risks, and expected outcomes of these interventions and help you make an informed decision regarding further treatment.
Lifestyle Changes and Home Remedies
Sometimes, making certain lifestyle modifications and home remedies can help alleviate the symptoms associated with glossopharyngeal nerve damage. These changes may include modifying the texture of food to aid swallowing, avoiding trigger foods that worsen symptoms, and staying well-hydrated.
It is important to consult with your healthcare provider before attempting any home remedies or lifestyle changes. They can provide tailored advice based on your specific circumstances and ensure that the proposed interventions align with your overall treatment plan.
Prognosis and Recovery from Glossopharyngeal Nerve Damage
Factors Influencing Recovery
The prognosis of glossopharyngeal nerve damage depends on various factors, including the underlying cause, severity of nerve injury, and individual patient characteristics. In cases of traumatic injury or surgical complications, recovery may be more challenging and may require longer rehabilitation periods.
Early diagnosis, prompt treatment, and adherence to a comprehensive management plan can significantly influence the recovery process. Your healthcare provider will monitor your progress and provide support throughout your journey to optimal health.
Coping and Support
Coping with glossopharyngeal nerve damage can be challenging, both physically and emotionally. It is essential to seek support from healthcare professionals, family, friends, or support groups that specialize in managing nerve damage or related conditions.
Additionally, strategies such as deep breathing exercises, meditation, and stress-management techniques may assist individuals in coping with the psychological and emotional impact of living with glossopharyngeal nerve damage.
Future Research and Developments
Ongoing advancements in medical research continue to enhance our understanding of glossopharyngeal nerve damage and its treatment options. Scientists and healthcare professionals are working collaboratively to develop innovative therapies, refine surgical techniques, and identify new diagnostic tools to optimize outcomes and patient satisfaction.
If you have been diagnosed with glossopharyngeal nerve damage, it is important to stay informed about developments in the field. Consult with your healthcare provider regularly to stay up to date with emerging treatment options and potential clinical trials that may offer new avenues for managing your condition.
In conclusion, glossopharyngeal nerve damage can occur due to trauma, medical conditions, or surgical interventions. The resulting symptoms can significantly impact an individual’s daily life. Early diagnosis, prompt treatment, and appropriate management strategies are essential for improving outcomes and enhancing overall well-being. If you suspect glossopharyngeal nerve damage, it is crucial to consult with a healthcare professional who can guide you through the diagnostic process and recommend the most suitable treatment plan for your specific needs.