The palatoglossal arch is a significant structure in the human body that plays a crucial role in various physiological functions. Understanding the anatomy and function of the palatoglossal arch can provide valuable insights into its relationship with the glossopharyngeal nerve, as well as shed light on the potential implications of anesthetizing this nerve.
Understanding the Palatoglossal Arch and Glossopharyngeal Nerve
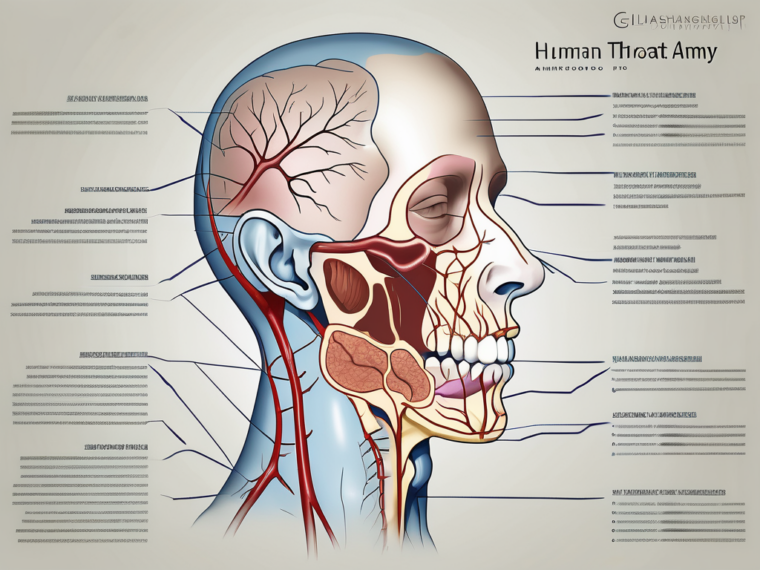
The palatoglossal arch is a fold of mucous membrane that connects the soft palate to the base of the tongue. It forms the boundary between the oral cavity and the oropharynx, serving as a protective barrier. The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves and provides sensory innervation to the oropharynx and posterior third of the tongue.
Anatomy of the Palatoglossal Arch
The palatoglossal arch is composed of muscular and fibrous tissues, and it extends from the soft palate to the base of the tongue, forming a spherical shape. The arch is created by the palatoglossus muscle, which arises from the palatine aponeurosis and courses downward to insert into the lateral posterior part of the tongue.
Within the palatoglossal arch, there is a complex network of blood vessels that supply oxygen and nutrients to the surrounding tissues. These blood vessels play a crucial role in maintaining the health and function of the palatoglossal arch. Additionally, the arch contains numerous sensory receptors, such as mechanoreceptors and nociceptors, which help in detecting pressure, touch, and pain sensations.
Furthermore, the palatoglossal arch is lined with specialized epithelial cells that secrete mucus. This mucus acts as a lubricant, facilitating the movement of food and saliva during swallowing. It also helps in protecting the underlying tissues from irritants and pathogens, contributing to the overall health of the oral cavity and oropharynx.
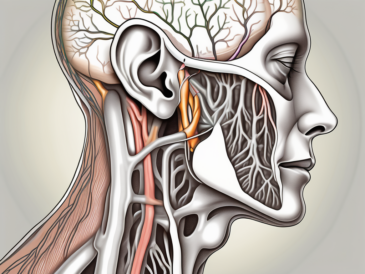
At the base of the palatoglossal arch lies a set of branches belonging to the glossopharyngeal nerve. These branches play a crucial role in the sensory innervation of the glossopharyngeal nerve and are significant targets for anesthetization when necessary. However, it is essential to understand the potential risks and complications associated with such procedures.
Structure and Function of the Glossopharyngeal Nerve
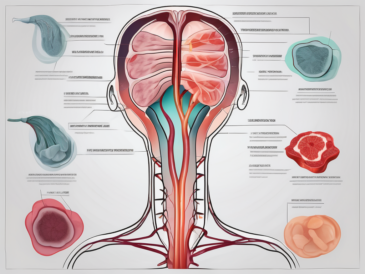
The glossopharyngeal nerve is a mixed nerve that originates from the medulla oblongata. It contains both motor and sensory fibers, making it a significant player in the oropharyngeal region. The sensory component of the glossopharyngeal nerve carries information from the posterior third of the tongue, tonsils, oropharynx, middle ear, and carotid sinus to the brain.
Within the glossopharyngeal nerve, there are specialized nerve endings called taste buds that are responsible for detecting different flavors. These taste buds are concentrated on the posterior third of the tongue, and they play a crucial role in our sense of taste. They send signals to the brain, allowing us to perceive and enjoy various flavors in the foods we consume.
The motor component of the glossopharyngeal nerve is responsible for innervating the stylopharyngeus muscle, which aids in swallowing and provides some sensation to the posterior tongue. This muscle contracts during the swallowing process, helping to propel food and liquids from the oral cavity into the esophagus. It also assists in the elevation of the larynx during swallowing, preventing food from entering the airway and causing choking.
Furthermore, the glossopharyngeal nerve plays a role in regulating blood pressure and heart rate. It contains specialized sensory receptors called baroreceptors, which detect changes in blood pressure. When these receptors sense a decrease in blood pressure, they send signals to the brain, resulting in the activation of mechanisms to increase blood pressure and maintain proper cardiovascular function.
The combined sensory and motor functions of the glossopharyngeal nerve are vital for the proper functioning of the oropharyngeal region. They allow us to perceive taste, swallow food, protect the airway, and maintain cardiovascular homeostasis. Understanding the intricate anatomy and functions of the palatoglossal arch and glossopharyngeal nerve is essential for healthcare professionals to diagnose and treat various conditions affecting these structures.
The Connection between Palatoglossal Arch and Glossopharyngeal Nerve
The palatoglossal arch and the glossopharyngeal nerve share a close anatomical relationship due to their proximity and intimate involvement in oropharyngeal functions. The structure of the palatoglossal arch serves as a pathway for the glossopharyngeal nerve branches, allowing for efficient sensory innervation of the oropharynx and posterior third of the tongue.
The palatoglossal arch, also known as the anterior tonsillar pillar, is a fold of mucous membrane that extends from the soft palate to the side of the tongue. It is composed of muscle fibers and connective tissue, providing support and stability to the oropharynx. This arch separates the oral cavity from the oropharynx and plays a crucial role in various physiological processes such as swallowing, speech production, and taste sensation.
The glossopharyngeal nerve, on the other hand, is one of the twelve cranial nerves and is responsible for providing sensory and motor innervation to the oropharynx and posterior third of the tongue. It originates from the medulla oblongata, the lower part of the brainstem, and travels through the skull to reach its target areas. The glossopharyngeal nerve carries taste information from the posterior third of the tongue, as well as general sensory information from the oropharynx.
How the Palatoglossal Arch Interacts with the Glossopharyngeal Nerve
The palatoglossal arch provides a supportive structure for the glossopharyngeal nerve branches as they pass through the oropharyngeal region. This interaction ensures proper sensory innervation and communication between the oropharynx, tongue, and the brain.
When the glossopharyngeal nerve branches reach the base of the palatoglossal arch, they continue their course to innervate specific areas of the oropharynx and posterior third of the tongue. This intricate connection allows for the transmission of sensory information, including taste perception and general sensation, to the brain.
However, it is important to note that anesthetizing the glossopharyngeal nerve branches at the base of the palatoglossal arch requires careful consideration and expertise. Administration of local anesthesia in this region may be useful in specific medical procedures but should only be done under the guidance and supervision of a trained medical professional.
The Role of the Palatoglossal Arch in Nerve Anesthetization
When conducting procedures that involve anesthetizing the glossopharyngeal nerve, targeting the branches located at the base of the palatoglossal arch may be considered. This can be achieved by carefully introducing the anesthetic agent into the specific area, ensuring precise and controlled administration.
By anesthetizing the glossopharyngeal nerve branches at the base of the palatoglossal arch, the transmission of sensory signals from the oropharynx and posterior third of the tongue to the brain can be temporarily blocked. This can be advantageous in certain medical procedures, such as tonsillectomies or biopsies, where reducing pain and discomfort is essential.
It is important to understand that anesthetizing the glossopharyngeal nerve branches at the base of the palatoglossal arch may result in temporary loss of sensation in the oropharynx and posterior third of the tongue. This can have potential implications, such as difficulty swallowing, altered taste perception, and changes in speech articulation. These effects are usually transient and resolve once the anesthesia wears off, but it highlights the importance of careful consideration and expertise when performing nerve anesthetization in this region.
Anesthetizing the Glossopharyngeal Nerve
Anesthetizing the glossopharyngeal nerve may be necessary in certain medical procedures such as dental surgeries, tonsillectomies, or other interventions involving the oropharyngeal region. However, the process of anesthetization should always be approached with caution and performed by qualified healthcare professionals with appropriate training and expertise.
The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a crucial role in the sensory and motor functions of the oropharynx. It provides sensation to the posterior third of the tongue, the tonsils, the soft palate, and the pharynx. Additionally, it contributes to the control of swallowing and taste perception.
The Process of Anesthetizing the Glossopharyngeal Nerve
The process of anesthetizing the glossopharyngeal nerve branches at the base of the palatoglossal arch involves the precise administration of local anesthesia. This can be achieved through various techniques, such as nerve blocks or direct injections, depending on the specific procedure and patient needs.
During a nerve block, the healthcare professional carefully identifies the location of the nerve branches and injects a local anesthetic agent to temporarily block the transmission of nerve signals. This effectively numbs the area and provides pain relief during the procedure.
On the other hand, direct injections involve the targeted delivery of local anesthesia to the specific nerve branches, ensuring accurate and localized numbing. This technique requires a high level of skill and knowledge of the anatomical structures involved.
It is important to highlight that the process of anesthetization should only be performed by trained healthcare professionals who have a deep understanding of the anatomical structures involved, potential risks, and proper administration techniques. They must also consider the patient’s medical history, allergies, and any potential contraindications.
Implications of Anesthetizing Different Branches of the Glossopharyngeal Nerve
When anesthetizing the glossopharyngeal nerve branches at the base of the palatoglossal arch, it is crucial to consider the potential implications and risks associated with this procedure. These may include temporary loss of sensation in the oropharynx, difficulties in swallowing, altered taste perception, or other sensory disturbances in the posterior third of the tongue.
Temporary loss of sensation in the oropharynx can affect the patient’s ability to perceive pain, temperature, and touch in the affected area. This can be advantageous during surgical procedures, as it allows the healthcare professional to work without causing discomfort to the patient. However, it is important to monitor the patient closely to ensure that the numbness does not lead to accidental injury, such as biting the tongue or the inside of the cheek.
Difficulties in swallowing, known as dysphagia, can occur due to the temporary disruption of the glossopharyngeal nerve’s motor function. This can cause discomfort and may require the patient to follow a modified diet or receive additional support, such as speech therapy, to regain normal swallowing function.
Altered taste perception is another potential side effect of anesthetizing the glossopharyngeal nerve. The nerve carries taste signals from the posterior third of the tongue to the brain, and its temporary blockage can lead to a distorted or diminished sense of taste. This can affect the patient’s enjoyment of food and beverages during the recovery period.
These potential side effects should be thoroughly discussed and evaluated with the patient prior to the procedure. It is important to have an open and honest conversation and obtain informed consent, ensuring the patient understands the benefits and risks associated with the anesthetization process.
Potential Risks and Complications
As with any medical intervention, anesthetizing the glossopharyngeal nerve branches at the base of the palatoglossal arch carries potential risks and complications that should be carefully considered and discussed with the patient. It is essential to prioritize patient safety and well-being throughout the entire process.
During the procedure, healthcare professionals must exercise caution to avoid any damage to surrounding structures, such as blood vessels or nerves. This requires a thorough understanding of the anatomical structures involved and the use of precise techniques and equipment. By adhering to strict procedural guidelines, the risk of complications can be minimized.
Furthermore, patients should be informed about the potential risks associated with glossopharyngeal nerve anesthetization. While rare, there is a possibility of infection at the injection site, bleeding, or allergic reactions to the anesthesia. These risks should be thoroughly explained to the patient, allowing them to make an informed decision about their treatment.
Possible Side Effects of Glossopharyngeal Nerve Anesthetization
The possible side effects of glossopharyngeal nerve anesthetization include temporary alterations in sensation and function in the oropharyngeal region. This can manifest as difficulties in swallowing, altered taste perception, temporary loss of sensation in the posterior third of the tongue, or other sensory disturbances.
Patients should be aware that these side effects are usually temporary and will resolve on their own within a few hours or days. However, it is important for patients to be prepared for the potential impact on their daily activities, such as eating, drinking, and speaking. They should be advised to follow any specific post-anesthetization instructions provided by their healthcare professional and report any unexpected or concerning symptoms.
It is worth noting that the occurrence of side effects can vary from person to person. Factors such as the individual’s overall health, the specific technique used during the procedure, and their body’s response to the anesthesia can all influence the likelihood and severity of side effects.
Precautions to Take When Anesthetizing the Glossopharyngeal Nerve
When anesthetizing the glossopharyngeal nerve branches at the base of the palatoglossal arch, it is crucial to adhere to strict procedural guidelines, ensuring patient safety and minimizing potential risks. Healthcare professionals should have a thorough understanding of the anatomical structures involved and utilize appropriate techniques and equipment.
Prior to the procedure, patients should undergo a comprehensive evaluation to assess their overall health and identify any potential contraindications. This evaluation may include a review of their medical history, allergies, and current medications. By considering these individual patient factors, healthcare professionals can ensure the safe and effective administration of anesthesia.
Furthermore, healthcare professionals should have a contingency plan in place to address any unexpected complications that may arise during the procedure. This may involve having the necessary equipment and medications readily available to manage potential allergic reactions, bleeding, or other adverse events.
By taking these precautions and closely monitoring the patient throughout the procedure, healthcare professionals can provide a safe and successful glossopharyngeal nerve anesthetization experience for their patients.
Recovery and Aftercare Post-Anesthetization
The recovery process following the anesthetization of the glossopharyngeal nerve branches at the base of the palatoglossal arch varies from patient to patient. It is important for healthcare professionals to provide comprehensive aftercare instructions and support to ensure a smooth recovery process.
What to Expect After Anesthetizing the Glossopharyngeal Nerve
Following the anesthetization of the glossopharyngeal nerve branches, patients may experience temporary alterations in sensation and function in the oropharyngeal region. These can include difficulties in swallowing, altered taste perception, or temporary loss of sensation in the posterior third of the tongue.
Patients should be advised to closely monitor their symptoms and report any unexpected or concerning changes to their healthcare professional. It is important to follow any post-anesthetization instructions provided, including any dietary restrictions or modifications that may be necessary during the recovery period.
Tips for a Smooth Recovery Process
To facilitate a smooth recovery process, patients should follow their healthcare professional’s instructions and recommendations. This may include adhering to a soft food, liquid, or modified diet for a prescribed period, practicing good oral hygiene, and avoiding specific activities or behaviors that could interfere with the healing process.
If patients experience any prolonged or concerning symptoms during their recovery, it is important to promptly seek medical attention and consult with the healthcare professional who performed the anesthetization procedure.
Conclusion
The base of the palatoglossal arch is an important anatomical location in the oropharyngeal region, closely associated with the glossopharyngeal nerve. Anesthetizing the branches of the glossopharyngeal nerve at this site can be beneficial for specific medical procedures; however, it should always be performed by trained healthcare professionals to ensure patient safety and minimize potential risks.
Prior to any procedure involving the anesthetization of the glossopharyngeal nerve, patients should be thoroughly informed of the benefits, risks, and potential side effects. Informed consent, open communication, and close follow-up care are essential elements in the management of patients undergoing glossopharyngeal nerve anesthetization.
As always, it is crucial to consult with a qualified healthcare professional to discuss individual medical conditions, treatment options, and potential risks prior to making any decisions regarding glossopharyngeal nerve anesthetization.