The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a crucial role in controlling various processes within the body. This intricate nerve is responsible for transmitting sensory and motor impulses to and from the throat, tongue, and certain vital organs, including the carotid sinus and the parotid gland. When the glossopharyngeal nerve is impacted, it can lead to a range of distressing symptoms and challenges for the affected individual.
Understanding the Glossopharyngeal Nerve
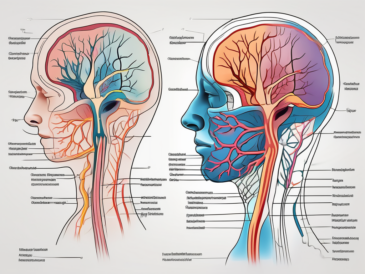
The glossopharyngeal nerve, originating from the brainstem, is one of the twelve cranial nerves that facilitate communication between the brain and various parts of the body. Classified as a mixed nerve, it comprises both sensory and motor fibers. These fibers enable the transmission of sensory information, such as taste and touch, from the back of the throat and posterior tongue to the brain. Additionally, the motor fibers control numerous vital functions, including swallowing, salivation, and speech articulation.
Anatomy of the Glossopharyngeal Nerve
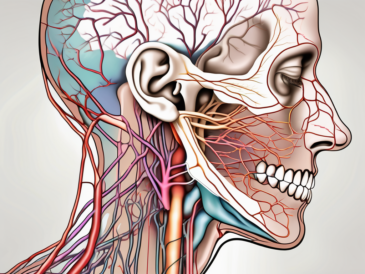
Structurally, the glossopharyngeal nerve emerges from the medulla oblongata, a region of the brainstem, and travels through several anatomical structures, including the jugular foramen. From its origin, the nerve branches out into various directions, connecting with different areas of the throat, tongue, and organs like the carotid sinus and parotid gland. This intricate network ensures the efficient transmission of neural signals throughout the body.
The glossopharyngeal nerve is composed of both sensory and motor fibers. The sensory fibers originate from the sensory ganglia located near the jugular foramen. These fibers receive sensory information from the posterior third of the tongue, the tonsils, the pharynx, and the carotid sinus. They transmit this information to the brain, allowing for the perception of taste, touch, and pain in these areas.
On the other hand, the motor fibers of the glossopharyngeal nerve arise from the nucleus ambiguus in the medulla oblongata. These fibers innervate the stylopharyngeus muscle, which plays a crucial role in swallowing and speech articulation. The motor fibers also contribute to the regulation of salivation by stimulating the parotid gland.
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve performs a range of essential functions that contribute to overall well-being. Some of these functions include taste perception at the back of the tongue, secretion of saliva, facilitation of swallowing, regulation of blood pressure and heart rate through connections with the carotid sinus, and involvement in the gag reflex. It is important to note that any impact on the glossopharyngeal nerve can result in significant disruptions to these functions.
One of the primary functions of the glossopharyngeal nerve is taste perception. The sensory fibers of the nerve carry taste information from the posterior third of the tongue to the brain. This allows us to differentiate between different flavors and enjoy the taste of food. Without the glossopharyngeal nerve, our ability to savor the deliciousness of various foods would be greatly diminished.
In addition to taste perception, the glossopharyngeal nerve is responsible for the secretion of saliva. The motor fibers of the nerve stimulate the parotid gland, which is one of the major salivary glands. Saliva plays a crucial role in the initial digestion of food, lubricating the mouth and facilitating the swallowing process. Without the glossopharyngeal nerve, our mouths would become dry, making it difficult to speak and swallow.
Speaking of swallowing, the glossopharyngeal nerve is also involved in this vital function. The motor fibers of the nerve innervate the stylopharyngeus muscle, which helps in the movement of the pharynx during swallowing. This coordinated muscular action ensures that food and liquids pass smoothly from the mouth to the esophagus, preventing choking and allowing for efficient digestion.
Furthermore, the glossopharyngeal nerve has connections with the carotid sinus, a specialized area in the carotid artery that helps regulate blood pressure and heart rate. The sensory fibers of the nerve receive information from the carotid sinus and transmit it to the brain. This allows for the appropriate adjustments in blood pressure and heart rate, ensuring that our cardiovascular system functions optimally.
Lastly, the glossopharyngeal nerve is involved in the gag reflex, a protective mechanism that helps prevent choking. When the back of the throat is stimulated, such as by an object touching the uvula or the back of the tongue, the sensory fibers of the glossopharyngeal nerve transmit this information to the brain. In response, the brain triggers a reflexive contraction of the muscles in the throat, causing a gagging sensation. This reflex helps expel any potential choking hazards and keeps our airways clear.
In conclusion, the glossopharyngeal nerve is a vital component of our nervous system, responsible for various functions that are essential for our well-being. From taste perception to saliva secretion, swallowing facilitation to blood pressure regulation, and involvement in the gag reflex, this nerve plays a crucial role in maintaining our overall health and ensuring the proper functioning of our body.
Causes of Glossopharyngeal Nerve Impact
There are several potential causes that can lead to the impact of the glossopharyngeal nerve. One common cause is physical injuries that affect the head, neck, or throat region. Trauma, such as motor vehicle accidents or falls, may result in compression or direct injury to the nerve. In addition to injuries, certain diseases and conditions can also impact the glossopharyngeal nerve, including tumors, infections, and neurological disorders.
Injuries Leading to Nerve Impact
Injuries to the head, neck, or throat region can exert pressure on the glossopharyngeal nerve, leading to its impact. This pressure may occur due to fractures, dislocations, or swelling. For example, a severe blow to the head during a car accident can cause the skull to fracture, potentially damaging the glossopharyngeal nerve in the process. Similarly, a fall from a significant height can result in neck injuries that affect the nerve’s function. Additionally, surgical procedures in the adjacent areas may inadvertently impact the nerve, causing temporary or persistent symptoms. It is important for healthcare professionals to consider these potential causes when evaluating patients with glossopharyngeal nerve impact.
Furthermore, sports-related injuries can also contribute to the impact of the glossopharyngeal nerve. Contact sports such as football or rugby pose a risk of head and neck injuries, which can potentially affect the nerve. Even non-contact sports like gymnastics or diving carry a risk of falls or collisions that can result in nerve damage. Coaches, trainers, and athletes should be aware of the potential consequences of these injuries and take appropriate precautions to minimize the risk.
Diseases and Conditions Affecting the Nerve
Various diseases and conditions can affect the glossopharyngeal nerve and lead to its impairment. Tumors, both benign and malignant, present in the head, neck, or throat region, can exert pressure on the nerve and disrupt its function. These tumors can arise from different tissues, such as the salivary glands, tongue, or throat, and their growth can gradually impinge on the glossopharyngeal nerve. Early detection and treatment of these tumors are crucial to prevent further nerve damage and complications.
Infections, such as abscesses or viral illnesses, can also impact the glossopharyngeal nerve, resulting in inflammation and subsequent symptoms. For instance, a severe throat infection, such as tonsillitis or pharyngitis, can spread to the surrounding tissues and affect the glossopharyngeal nerve. The body’s immune response to the infection can cause swelling and irritation, leading to compression of the nerve. Prompt medical intervention, including appropriate antibiotics or antiviral medications, is necessary to control the infection and minimize nerve damage.
Additionally, certain neurological disorders, including multiple sclerosis, can affect the glossopharyngeal nerve as part of a more widespread dysfunction in the nervous system. Multiple sclerosis is an autoimmune disease that causes the immune system to mistakenly attack the protective covering of nerve fibers, known as myelin. This demyelination process can affect various nerves in the body, including the glossopharyngeal nerve, leading to impaired function. Managing the underlying neurological condition is essential in preventing further damage to the nerve and maintaining overall neurological health.
Moreover, certain lifestyle factors can contribute to the impact of the glossopharyngeal nerve. Chronic alcohol consumption, for example, can lead to nutritional deficiencies, including thiamine deficiency, which can affect the nerves, including the glossopharyngeal nerve. Similarly, smoking can impair blood flow to the nerves, potentially compromising their function. Adopting a healthy lifestyle, including a balanced diet and avoiding harmful habits, can help minimize the risk of nerve damage.
Symptoms of Glossopharyngeal Nerve Impact
A patient with an impacted glossopharyngeal nerve may experience a range of distressing symptoms, both physical and functional. These symptoms may vary depending on the specific area of nerve involvement and the extent of the impact.
The glossopharyngeal nerve, also known as the ninth cranial nerve, is responsible for providing sensation to the back of the throat, tongue, and parts of the ear. It also plays a crucial role in taste perception, swallowing, and controlling the muscles involved in speech articulation.
Physical Symptoms and Discomfort
Patients with glossopharyngeal nerve impact may complain of severe pain in the back of the throat, ears, or tongue region. This pain may be sharp or throbbing in nature and can significantly interfere with daily activities and quality of life. In some cases, the pain may radiate to the jaw or neck.
In addition to pain, individuals may experience difficulty opening their mouths fully, leading to challenges with eating, speaking, or even breathing. This limitation in mouth opening, known as trismus, can be caused by muscle spasms or weakness resulting from the nerve impact.
Furthermore, the impacted glossopharyngeal nerve can cause a sensation of a lump or foreign object in the throat, known as globus pharyngeus. This sensation can be distressing and may lead to anxiety or difficulty swallowing.
Changes in Taste and Swallowing
Due to the involvement of the glossopharyngeal nerve in taste perception and swallowing, patients may report alterations in their ability to taste certain flavors or swallowing difficulties.
Changes in taste perception can range from a diminished sense of taste to a complete loss of taste in certain regions of the tongue. This can affect the enjoyment of food and may lead to a decreased appetite or changes in dietary preferences.
Moreover, swallowing challenges may manifest as a sensation of food getting stuck in the throat, recurrent choking episodes, or even aspiration. Aspiration occurs when food or liquid enters the airway instead of the esophagus, which can lead to respiratory problems and increase the risk of pneumonia.
These symptoms can have a significant impact on a person’s nutritional status and overall well-being. It is important for individuals experiencing taste and swallowing difficulties to seek medical attention for proper evaluation and management.
Voice and Speech Alterations
The glossopharyngeal nerve plays a crucial role in controlling the muscles involved in speech articulation. Therefore, individuals impacted by this nerve may experience alterations in their voice quality and speech patterns.
This can manifest as a hoarse or weak voice, difficulty pronouncing certain sounds or words, or general slurring of speech. These changes in voice and speech can significantly impact an individual’s ability to communicate effectively, necessitating intervention and therapy.
In some cases, the impact on the glossopharyngeal nerve may also affect the muscles responsible for swallowing and breathing coordination, leading to further speech difficulties and respiratory problems.
Speech therapy, along with other interventions, may be recommended to help patients regain their speech abilities and improve their overall quality of life.
Diagnostic Procedures for Glossopharyngeal Nerve Impact
When diagnosing glossopharyngeal nerve impact, healthcare professionals rely on various diagnostic procedures to assess the nerve’s function and identify the underlying cause of the impairment.
The diagnostic process begins with a comprehensive medical history, where the healthcare professional gathers detailed information about the patient’s symptoms and medical background. This includes asking questions about the nature and duration of the symptoms, any previous medical conditions or surgeries, and any family history of neurological disorders. The medical history is crucial in determining the potential impact on the glossopharyngeal nerve and helps guide further diagnostic steps.
Following the medical history, a thorough physical examination is conducted, with a particular focus on the head, neck, and throat regions. The healthcare professional carefully examines these areas, looking for any visible abnormalities, such as swelling, redness, or lesions. They may also palpate the neck and throat to check for tenderness or enlarged lymph nodes. This physical examination helps identify any external signs that may be related to glossopharyngeal nerve impact.
In some cases, healthcare professionals may order imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, to confirm or rule out physical damage to the nerve. These non-invasive tests provide detailed images of the head, neck, and throat regions, allowing healthcare professionals to identify any structural abnormalities or potential sources of nerve compression. MRI scans use powerful magnets and radio waves to create detailed images, while CT scans use X-rays and computer technology to produce cross-sectional images. These imaging tests can help visualize the glossopharyngeal nerve and surrounding structures, aiding in the diagnosis process.
Additionally, laboratory tests may be conducted to investigate potential underlying conditions that could be impacting the glossopharyngeal nerve. Blood tests can help identify infections, such as viral or bacterial infections, that may be causing nerve inflammation or damage. Other laboratory tests may be performed to assess the patient’s overall health and screen for systemic illnesses that could contribute to nerve impairment. These tests provide valuable information to healthcare professionals, aiding in the identification of the underlying cause of glossopharyngeal nerve impact.
Treatment Options for Glossopharyngeal Nerve Impact
Effective management of glossopharyngeal nerve impact depends on the underlying cause and the extent of nerve involvement. Treatment approaches primarily aim to alleviate symptoms, improve function, and address the root cause of the impairment.
Medications and Therapies
In cases where infections or inflammatory conditions impact the glossopharyngeal nerve, doctors may prescribe appropriate medications, such as antibiotics or corticosteroids, to reduce inflammation and promote healing. Physical therapy and speech therapy may also be beneficial in restoring muscle strength, improving swallowing function, and enhancing voice and communication skills.
Surgical Interventions
In certain cases, surgical intervention may be necessary to alleviate nerve compression or remove tumors that impede the function of the glossopharyngeal nerve. These procedures are typically performed by skilled neurosurgeons or otolaryngologists and require a thorough evaluation of the risks and potential benefits.
Prognosis and Recovery from Glossopharyngeal Nerve Impact
The prognosis for patients with glossopharyngeal nerve impact varies depending on the underlying cause, severity of nerve damage, and timely intervention. While some individuals may experience a full recovery with appropriate treatment and rehabilitation, others may face long-term challenges and require ongoing management.
Expected Recovery Timeline
The recovery timeline for glossopharyngeal nerve impact depends on multiple factors, including the extent of nerve damage, the underlying cause, and the effectiveness of treatment. In cases where nerve compression or inflammation is promptly addressed, gradual improvement in symptoms can be expected within a few weeks to months. However, where structural damage or irreversible nerve dysfunction exists, long-term management strategies may be necessary to optimize function and well-being.
Long-term Health Considerations
Individuals impacted by glossopharyngeal nerve dysfunction should prioritize ongoing medical consultations to ensure optimal management and monitor any potential complications or long-term health considerations. Consulting with a healthcare professional who specializes in neurology or otolaryngology can provide valuable guidance in navigating the challenges associated with glossopharyngeal nerve impact.
In conclusion, glossopharyngeal nerve impact can result in a range of distressing symptoms and functional challenges for affected individuals. Prompt medical attention, accurate diagnosis, and appropriate treatment interventions are critical. If you or someone you know experiences any symptoms suggestive of glossopharyngeal nerve impact, it is essential to seek medical advice and consultation for a thorough evaluation and individualized management plan.