The glossopharyngeal nerve is a crucial cranial nerve that plays a vital role in various functions of the body, including swallowing, taste sensation, and the monitoring of blood pressure. When this nerve is affected by a disorder, it can lead to a range of symptoms and complications. In this article, we will explore the different aspects of the glossopharyngeal nerve, common disorders associated with it, symptoms indicating a problem, diagnostic procedures, treatment options, and prevention strategies.
Understanding the Glossopharyngeal Nerve
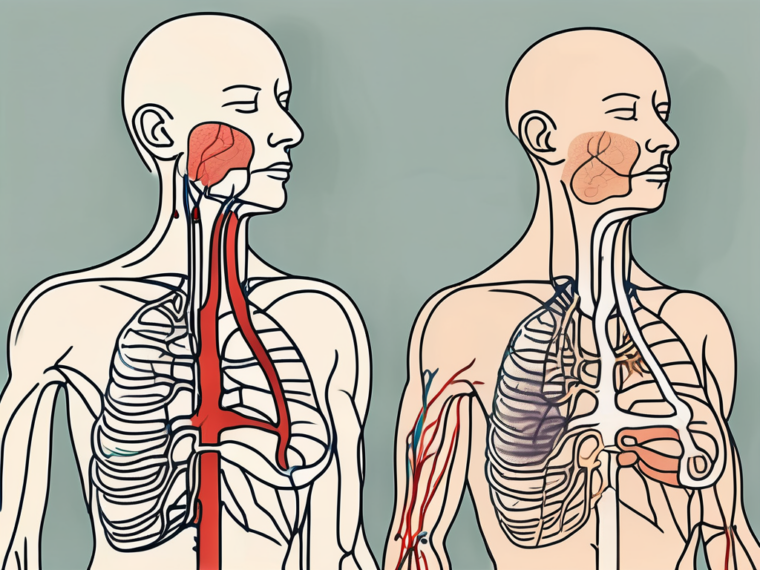
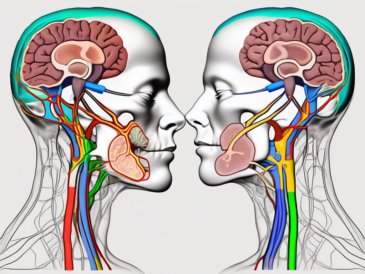
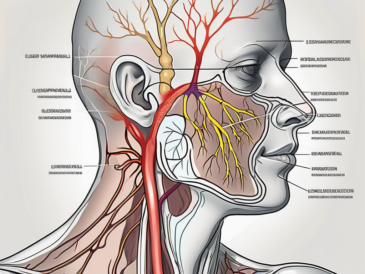
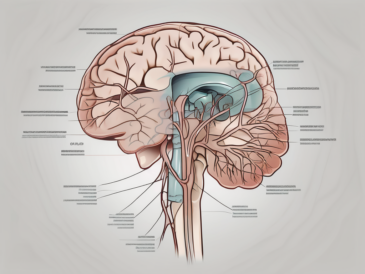
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves originating from the brainstem. It consists of both sensory and motor fibers, which allow it to perform multiple functions. The sensory fibers of the glossopharyngeal nerve transmit information from the back of the throat, tongue, and ear to the brain. On the other hand, the motor fibers control the muscles involved in swallowing.
The anatomy of the glossopharyngeal nerve is fascinating. It arises from the medulla oblongata, the lower part of the brainstem, and exits the skull through the jugular foramen. From there, it branches out and innervates various structures in the head and neck region. One of its branches, known as the tympanic nerve, passes through the middle ear and provides sensory innervation to the eardrum and the mucous membrane of the middle ear.
Anatomy of the Glossopharyngeal Nerve
The glossopharyngeal nerve is not only responsible for transmitting sensory information but also plays a crucial role in motor functions. Its motor fibers innervate the stylopharyngeus muscle, which is involved in the process of swallowing. This muscle helps elevate the pharynx during swallowing, allowing food and liquids to pass through the throat and into the esophagus.
Furthermore, the glossopharyngeal nerve has a unique connection to the parotid gland, a major salivary gland located in front of the ear. It carries parasympathetic fibers that stimulate the production of saliva, aiding in the digestion of food and maintaining oral health.
Function of the Glossopharyngeal Nerve
The glossopharyngeal nerve serves several crucial functions in the body. One of its primary roles is to contribute to the complex process of swallowing by coordinating the movements of the throat muscles. Without the glossopharyngeal nerve, swallowing would be difficult and inefficient.
In addition to its role in swallowing, the glossopharyngeal nerve is responsible for carrying taste sensations from the back of the tongue. It allows us to perceive the flavors of food and beverages, enhancing our overall sensory experience during meals.
Another fascinating function of the glossopharyngeal nerve is its involvement in monitoring blood pressure levels. Specialized sensory receptors called baroreceptors are located in the walls of certain blood vessels, particularly in the carotid sinus and aortic arch. These baroreceptors detect changes in blood pressure and send signals through the glossopharyngeal nerve to the brain, which then initiates appropriate adjustments to maintain blood pressure within a healthy range.
Furthermore, the glossopharyngeal nerve plays a role in regulating saliva production. Through its parasympathetic fibers, it stimulates the release of saliva from the parotid gland. Saliva not only aids in digestion but also helps keep the oral cavity moist, protecting the teeth and gums from infections and maintaining overall oral health.
Common Disorders of the Glossopharyngeal Nerve
Glossopharyngeal Neuralgia
Glossopharyngeal neuralgia is a rare condition characterized by intense, recurring pain in the back of the throat, tongue, tonsillar area, or ear. It can be triggered by various activities, such as swallowing, talking, or even touching the affected areas. This condition is often caused by compression or irritation of the glossopharyngeal nerve, potentially due to conditions like blood vessel abnormalities or tumors.
The pain experienced in glossopharyngeal neuralgia can be excruciating and debilitating, often described as sharp, stabbing, or electric shock-like. It may last for a few seconds to a few minutes, and can occur multiple times throughout the day. The episodes of pain can be triggered by simple actions like eating, drinking, or even speaking.
Diagnosing glossopharyngeal neuralgia can be challenging, as the symptoms may overlap with other conditions such as dental problems or ear infections. However, a thorough medical history, physical examination, and imaging tests like MRI or CT scans can help in identifying the underlying cause and confirming the diagnosis.
Treatment options for glossopharyngeal neuralgia include medications to manage pain, such as anticonvulsants or tricyclic antidepressants. In some cases, surgical interventions like microvascular decompression or nerve blocks may be considered to relieve the compression or irritation of the glossopharyngeal nerve.
Glossopharyngeal Nerve Palsy
Glossopharyngeal nerve palsy refers to the weakness or paralysis of the muscles controlled by the glossopharyngeal nerve, primarily the muscles involved in swallowing. This condition can result in difficulties in swallowing, which can lead to aspiration or malnutrition if not properly managed. The causes of glossopharyngeal nerve palsy can range from infections to trauma or tumors affecting the nerve.
When glossopharyngeal nerve palsy occurs, individuals may experience symptoms such as difficulty swallowing solids or liquids, choking or coughing while eating, and a sensation of food getting stuck in the throat. They may also have a weak or hoarse voice, as the glossopharyngeal nerve also plays a role in controlling the muscles involved in speech.
Diagnosing glossopharyngeal nerve palsy involves a comprehensive evaluation of the individual’s medical history, physical examination, and potentially additional tests like electromyography (EMG) or imaging studies. Identifying the underlying cause is crucial in determining the appropriate treatment approach.
Treatment for glossopharyngeal nerve palsy focuses on managing the symptoms and addressing the underlying cause. This may involve speech therapy to improve swallowing function, dietary modifications to ensure adequate nutrition, and medications to relieve pain or reduce inflammation. In some cases, surgical intervention may be necessary to repair or remove any structures compressing the glossopharyngeal nerve.
Rehabilitation and support from a multidisciplinary team, including speech therapists, dieticians, and neurologists, can greatly improve the quality of life for individuals with glossopharyngeal nerve palsy. With proper management and treatment, many individuals are able to regain normal swallowing function and alleviate associated symptoms.
Symptoms Indicating a Problem with the Glossopharyngeal Nerve
The glossopharyngeal nerve is a crucial component of the human nervous system, responsible for various functions related to swallowing, speech, and sensory perception. When this nerve is affected by a disorder or injury, it can manifest in a range of physical and sensory symptoms, which can greatly impact an individual’s quality of life.
Physical Symptoms
One of the most common physical symptoms associated with glossopharyngeal nerve dysfunction is difficulty swallowing, also known as dysphagia. This can make it challenging for individuals to consume food and liquids, leading to weight loss, malnutrition, and dehydration if left untreated.
In addition to difficulty swallowing, patients may experience a persistent sensation of something stuck in the throat, known as globus pharyngeus. This sensation can be extremely distressing and may cause anxiety and discomfort, as individuals constantly feel the need to clear their throat.
Hoarseness and voice changes are also common physical symptoms of glossopharyngeal nerve problems. The nerve plays a crucial role in controlling the muscles responsible for vocalization, and any disruption can lead to changes in voice quality, pitch, and volume.
Furthermore, patients with glossopharyngeal nerve dysfunction may experience a persistent sore throat, which can be accompanied by pain in the back of the throat or tongue. These symptoms can make it uncomfortable to speak, eat, or even breathe, significantly impacting an individual’s daily activities and overall well-being.
Sensory Symptoms
In addition to the physical symptoms mentioned above, disorders of the glossopharyngeal nerve can also result in sensory abnormalities. One of the most notable sensory symptoms is altered taste sensations, particularly at the back of the tongue. Patients may report a metallic or bitter taste, which can affect their enjoyment of food and beverages.
The glossopharyngeal nerve also plays a crucial role in the gag reflex, which helps protect the airway from foreign objects. When this nerve is affected, individuals may experience a decreased or altered gag reflex. This can make it difficult for them to swallow safely and increase the risk of choking or aspiration.
It is important to note that the symptoms mentioned above are not exhaustive, and the presentation of glossopharyngeal nerve dysfunction can vary from person to person. Some individuals may only experience a few of these symptoms, while others may have a combination of physical and sensory manifestations.
If you suspect you may have a problem with your glossopharyngeal nerve, it is crucial to seek medical attention for a proper diagnosis and appropriate treatment. Early intervention can help manage symptoms effectively and improve overall quality of life.
Diagnostic Procedures for Glossopharyngeal Nerve Disorders
Medical History and Physical Examination
When evaluating a potential glossopharyngeal nerve disorder, a healthcare professional will typically begin by gathering a detailed medical history. This information can help identify potential risk factors or underlying conditions contributing to the symptoms. For example, the healthcare professional may inquire about the patient’s history of throat infections, head or neck trauma, or any previous surgeries in the area. Additionally, they may ask about any symptoms the patient is experiencing, such as difficulty swallowing, pain in the throat or ear, or changes in taste sensation.
After obtaining the medical history, a thorough physical examination will be conducted to assess the patient’s throat muscles, reflexes, and sensation. The healthcare professional may use a tongue depressor to examine the back of the throat and check for any abnormalities or signs of inflammation. They may also gently touch different areas of the throat to assess the patient’s sensation and determine if there are any areas of numbness or hypersensitivity.
Imaging Tests
Imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be recommended to get a more detailed view of the glossopharyngeal nerve, as well as surrounding structures. These tests can help identify any structural abnormalities, tumors, or other factors potentially impacting the nerve’s function. During an MRI, the patient will lie on a table that slides into a large, cylindrical machine. The machine uses a magnetic field and radio waves to create detailed images of the throat and surrounding areas. CT scans, on the other hand, use a series of X-ray images taken from different angles to create cross-sectional images of the throat.
Prior to undergoing these imaging tests, the patient may be asked to remove any jewelry or metal objects that could interfere with the imaging process. They may also be given a contrast dye to enhance the visibility of certain structures or abnormalities. The imaging tests themselves are painless, but some patients may experience mild discomfort from lying still for an extended period of time.
Nerve Conduction Studies
Nerve conduction studies involve measuring the electrical activity of the glossopharyngeal nerve. This test can help determine whether there is any damage or disruption in the nerve’s ability to transmit signals. During the procedure, small electrodes are placed on the skin overlying the nerve. A mild electrical stimulus is then applied to the nerve, and the resulting electrical activity is recorded and analyzed.
Additionally, electromyography (EMG) may be conducted to evaluate the function of the muscles controlled by the glossopharyngeal nerve. This test involves inserting a thin needle electrode into the muscle to measure its electrical activity at rest and during contraction. By assessing the muscle’s response to electrical stimulation, the healthcare professional can gain insight into the nerve-muscle connection and identify any abnormalities or dysfunction.
Both nerve conduction studies and electromyography are typically well-tolerated by patients, although some may experience mild discomfort or temporary muscle twitching during the procedure.
Treatment Options for Glossopharyngeal Nerve Disorders
The glossopharyngeal nerve is a crucial component of the nervous system, responsible for transmitting sensory information from the tongue, throat, and surrounding areas to the brain. When this nerve becomes disordered, it can lead to a range of symptoms and discomfort. Fortunately, there are several treatment options available to manage glossopharyngeal nerve disorders and alleviate associated pain.
Medication Therapies
Depending on the specific glossopharyngeal nerve disorder, various medications may be prescribed to manage symptoms and reduce pain. For glossopharyngeal neuralgia, anticonvulsant medications or tricyclic antidepressants may be used to alleviate pain episodes. These medications work by targeting the nerve impulses and reducing their intensity, providing relief to individuals suffering from this condition.
In cases where glossopharyngeal nerve palsy is the primary concern, non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants may be prescribed. These medications help to relieve muscle spasticity associated with the disorder, allowing for improved coordination and reduced discomfort.
Surgical Interventions
In some cases, surgical interventions may be necessary, particularly if conservative treatments do not provide sufficient relief. Surgical options could include microvascular decompression, which involves relieving pressure on the glossopharyngeal nerve caused by blood vessels or other structures. This procedure aims to alleviate the compression and restore normal nerve function.
Other surgical procedures may be performed to remove tumors that may be affecting the glossopharyngeal nerve. Additionally, surgical interventions can be used to repair nerve damage or address underlying causes of the disorder, providing long-term relief and improving overall quality of life.
Alternative Therapies
Complementary and alternative therapies can also play a role in the management of glossopharyngeal nerve disorders. Physiotherapy, for example, focuses on improving muscle coordination and strength, which can help alleviate symptoms associated with glossopharyngeal nerve palsy.
Acupuncture, a traditional Chinese medicine practice, has also shown promise in reducing pain and promoting overall well-being. By targeting specific points on the body, acupuncture can help stimulate the release of endorphins, which are natural pain-relieving chemicals.
Biofeedback, another alternative therapy, involves using electronic devices to monitor and provide feedback on physiological processes such as muscle tension and heart rate. By learning to control these processes, individuals with glossopharyngeal nerve disorders can effectively manage their symptoms and improve their overall well-being.
It is important to note that while alternative therapies can be beneficial, it is crucial to consult with a healthcare professional before beginning any of these treatment approaches. They can provide guidance and ensure that these therapies are safe and suitable for individual needs.
Prevention and Management of Glossopharyngeal Nerve Disorders
Lifestyle Changes
While it may not be possible to prevent all glossopharyngeal nerve disorders, certain lifestyle modifications can contribute to overall nerve health and minimize the risk of complications. These may include maintaining a healthy diet to support nerve function, practicing good oral hygiene, avoiding excessive alcohol consumption, and quitting smoking. Additionally, stress management techniques and regular exercise can promote overall well-being and reduce the risk of certain nerve-related conditions.
Regular Check-ups and Monitoring
For individuals with glossopharyngeal nerve disorders, regular check-ups and monitoring are essential. This allows healthcare professionals to assess the progress of the condition, adjust treatment plans if necessary, and provide ongoing support and guidance. It is important to promptly report any new or worsening symptoms to ensure timely intervention and prevention of potential complications.
Coping Strategies for Living with a Glossopharyngeal Nerve Disorder
Living with a glossopharyngeal nerve disorder can be challenging, both physically and emotionally. It is crucial for individuals to develop coping strategies to manage the impact of the condition on their daily lives. This may involve working closely with healthcare professionals, joining support groups or seeking counseling, and exploring relaxation techniques to alleviate stress and enhance overall well-being.
In conclusion, the glossopharyngeal nerve plays a critical role in various bodily functions, and when it malfunctions or becomes affected by disorders, it can result in significant symptoms and complications. If you suspect you may have a problem with your glossopharyngeal nerve, it is essential to consult with a healthcare professional for a comprehensive evaluation and appropriate management. Remember, early detection and intervention can greatly improve outcomes and quality of life for individuals with glossopharyngeal nerve disorders.