The glossopharyngeal nerve, also known as cranial nerve IX, plays a vital role in the functioning of the human body. This article aims to provide a comprehensive understanding of the glossopharyngeal nerve, including its anatomy, functions, associated disorders, diagnostic procedures, treatment options, and future research prospects.
Understanding the Glossopharyngeal Nerve
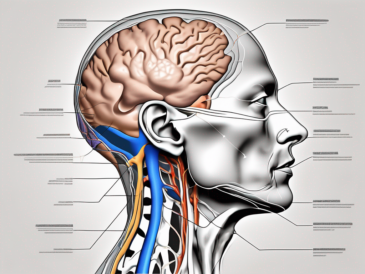
Before delving into the functions and complexities of the glossopharyngeal nerve, it is essential to comprehend its anatomy. The glossopharyngeal nerve is one of the 12 cranial nerves originating from the brainstem. It arises from the medulla oblongata, specifically the posterior aspect, and extends downwards through the neck and throat region.
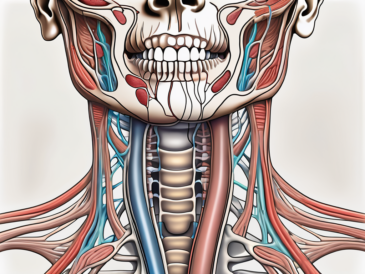
The nerve consists of both sensory and motor fibers. The sensory fibers are responsible for transmitting signals from the back of the tongue, tonsils, and the throat to the brain, while the motor fibers control the movement of certain muscles involved in swallowing and speech production.
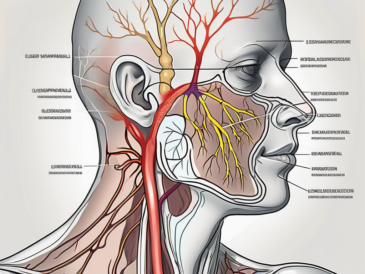
Understanding the anatomy of the glossopharyngeal nerve provides insight into its intricate functions. The nerve is not a singular entity but rather a complex network of branches that innervate different areas of the head and neck region. These branches include the tympanic nerve, carotid sinus nerve, and stylopharyngeal nerve, among others. Each branch serves specific functions, allowing for precise coordination of sensory and motor activities.
Anatomy of the Glossopharyngeal Nerve
The tympanic nerve, a branch of the glossopharyngeal nerve, plays a crucial role in the auditory system. It carries sensory information from the middle ear to the brain, allowing us to perceive sound and maintain balance. Without the glossopharyngeal nerve’s involvement, our ability to hear and maintain equilibrium would be compromised.
The carotid sinus nerve, another branch of the glossopharyngeal nerve, is responsible for monitoring blood pressure in the carotid sinus. This specialized structure, located in the neck, detects changes in blood pressure and sends signals to the brainstem for appropriate adjustments. The glossopharyngeal nerve’s connection to the carotid sinus ensures that our bodies can regulate blood pressure effectively.
One of the most significant branches of the glossopharyngeal nerve is the stylopharyngeal nerve. This branch innervates the stylopharyngeus muscle, which plays a vital role in swallowing and speech production. Without the glossopharyngeal nerve’s motor fibers controlling the movement of the stylopharyngeus muscle, these essential functions would be impaired.
The Nerve’s Connection to the Brainstem
The glossopharyngeal nerve has a close association with the brainstem, making it an integral part of the central nervous system. Its connection to the medulla oblongata allows for bidirectional communication between the brain and various structures innervated by the nerve. This connection plays a crucial role in coordinating the nerve’s functions with other bodily processes.
Furthermore, the glossopharyngeal nerve’s connection to the brainstem enables it to interact with other cranial nerves, such as the vagus nerve. This interaction allows for the seamless coordination of complex functions, including swallowing, speech, and regulation of blood pressure.
In conclusion, the glossopharyngeal nerve is a remarkable structure with multifaceted functions. Its intricate anatomy, consisting of various branches, ensures precise coordination of sensory and motor activities in the head and neck region. The nerve’s connection to the brainstem further enhances its role in maintaining essential bodily processes. Understanding the complexities of the glossopharyngeal nerve provides valuable insights into the intricate workings of the human body.
Detailed Functions of the Glossopharyngeal Nerve
Now that we have explored the anatomy and connection of the glossopharyngeal nerve, let us delve into its specific functions.
The glossopharyngeal nerve, also known as the ninth cranial nerve, is a crucial component of the human nervous system. It is responsible for a variety of important functions that are essential for our daily lives.
Role in Taste Sensation
The glossopharyngeal nerve carries sensory information related to taste perception from the back of the tongue. It allows us to savor the diverse flavors of food and beverages. This remarkable nerve enables us to distinguish between sweet, sour, salty, and bitter tastes, enhancing our overall culinary experience. Without the glossopharyngeal nerve, our ability to appreciate the intricate flavors in our favorite dishes would be greatly diminished.
Moreover, the glossopharyngeal nerve’s involvement in taste sensation extends beyond mere pleasure. It also serves as a protective mechanism, as it helps us identify potentially harmful substances. For instance, when we accidentally consume something spoiled or toxic, the glossopharyngeal nerve triggers an immediate aversive response, causing us to spit out the offending substance and avoid further harm.
Its Part in Swallowing and Speech
The motor fibers of the glossopharyngeal nerve contribute to the vital processes of swallowing and speech production. These fibers coordinate the movement of muscles involved in these activities, ensuring their smooth execution. Without the glossopharyngeal nerve’s motor function, these seemingly effortless actions would become arduous tasks.
When we swallow, the glossopharyngeal nerve plays a crucial role in coordinating the precise sequence of muscle contractions required to propel food and liquids from the mouth to the esophagus. This intricate process involves the activation of various muscles, including those in the throat and the upper esophagus. The glossopharyngeal nerve ensures that these muscles contract in perfect harmony, allowing us to effortlessly consume and digest our meals.
In addition to swallowing, the glossopharyngeal nerve is also involved in speech production. It controls the movement of the muscles responsible for articulating sounds and forming words. Without the precise coordination provided by the glossopharyngeal nerve, our ability to communicate effectively through speech would be severely impaired.
Contribution to Salivation
The glossopharyngeal nerve also plays a vital role in stimulating salivary gland secretion. It activates the parotid gland, one of the major salivary glands responsible for moistening the mouth and aiding in digestion. The parotid gland produces saliva, a fluid that contains enzymes necessary for breaking down food particles and initiating the digestive process.
When we eat, the glossopharyngeal nerve triggers the release of saliva, ensuring that our food is adequately moistened and prepared for digestion. This process not only facilitates the mechanical breakdown of food but also enhances our ability to taste and enjoy the flavors of different cuisines.
Furthermore, saliva plays a crucial role in maintaining oral health. It helps to neutralize acids produced by bacteria, preventing tooth decay and gum disease. Additionally, saliva contains antibacterial properties that help to keep the oral cavity clean and free from harmful microorganisms.
Damage to the glossopharyngeal nerve can have significant consequences. Reduced salivary production, known as xerostomia or dry mouth, can lead to difficulties in speaking, swallowing, and even tasting food. It can also increase the risk of dental problems and oral infections.
In conclusion, the glossopharyngeal nerve is a multifunctional nerve that plays a vital role in taste sensation, swallowing, speech production, and salivation. Its intricate network of sensory and motor fibers ensures the seamless coordination of various processes necessary for our overall well-being. Understanding the detailed functions of the glossopharyngeal nerve allows us to appreciate its significance in our daily lives and underscores the importance of maintaining its health and functionality.
Disorders Associated with the Glossopharyngeal Nerve
The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a crucial role in the functioning of the throat, tongue, and ear. However, this important nerve is susceptible to various disorders that can disrupt its normal operation.
One common disorder associated with the glossopharyngeal nerve is glossopharyngeal neuralgia. Glossopharyngeal neuralgia refers to recurrent episodes of severe pain in the throat, tongue, and ear. This excruciating discomfort often occurs due to irritation or compression of the glossopharyngeal nerve. If you experience persistent or worsening throat pain, it is important to consult a healthcare professional to rule out potential glossopharyngeal neuralgia.
Implications of damage to the glossopharyngeal nerve can be far-reaching. Damage to this nerve can result from various causes, such as trauma, infections, or underlying medical conditions. Depending on the extent of the damage, individuals may experience difficulty with swallowing, speech, taste perception, and salivation.
Swallowing difficulties, known as dysphagia, can significantly impact an individual’s quality of life. It can lead to malnutrition, dehydration, and weight loss. Speech difficulties, on the other hand, can affect communication and social interactions. Taste perception abnormalities can make it challenging to enjoy food and beverages, while reduced salivation can cause dry mouth and oral health problems.
Seeking prompt medical attention is crucial in cases of glossopharyngeal nerve damage. A thorough evaluation by a healthcare professional can help determine the underlying cause and initiate appropriate treatment. Treatment options may include medication to manage pain and inflammation, physical therapy to improve swallowing and speech, and in some cases, surgical intervention to relieve compression on the nerve.
Diagnostic Procedures for Glossopharyngeal Nerve Issues
When individuals present with symptoms potentially related to glossopharyngeal nerve dysfunction, healthcare professionals may employ specific diagnostic procedures to assess the condition accurately.
The glossopharyngeal nerve is a cranial nerve that plays a crucial role in various functions, including swallowing, taste sensation in the posterior third of the tongue, and the gag reflex. Dysfunction of this nerve can lead to a range of symptoms, such as difficulty swallowing, altered taste perception, and throat pain.
Physical Examination
A thorough physical examination is often the first step in evaluating glossopharyngeal nerve issues. Healthcare providers may assess sensory and motor functions by examining the tongue, throat, and other relevant areas. They will carefully observe the patient’s ability to swallow, looking for any signs of aspiration or difficulty in moving food from the mouth to the esophagus.
During the physical examination, healthcare professionals may also perform tests to evaluate the patient’s taste sensation. This can involve using taste strips or solutions with different flavors to determine if there is any impairment in the posterior third of the tongue, which is innervated by the glossopharyngeal nerve.
Additionally, they may inquire about symptoms and medical history to gain insight into potential underlying causes. Certain medical conditions, such as diabetes or viral infections like herpes zoster, can affect the glossopharyngeal nerve and lead to dysfunction.
Imaging Techniques
In some cases, diagnostic imaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be necessary to visualize the structures associated with the glossopharyngeal nerve. These imaging techniques can help identify potential compressions, lesions, or abnormalities that could be contributing to nerve dysfunction.
An MRI scan provides detailed images of the soft tissues, allowing healthcare professionals to assess the anatomy of the glossopharyngeal nerve and surrounding structures. It can help identify any tumors, cysts, or other abnormalities that may be affecting the nerve’s function.
On the other hand, a CT scan uses X-rays to create cross-sectional images of the head and neck region. It can be particularly useful in detecting bony abnormalities or calcifications that may be compressing the glossopharyngeal nerve.
During these imaging procedures, patients will lie on a table that slides into a large, tunnel-like machine. It is essential to remain still during the scan to ensure accurate and clear images. In some cases, a contrast dye may be injected to enhance the visibility of certain structures or abnormalities.
Once the diagnostic procedures are complete, healthcare professionals can analyze the findings to determine the underlying cause of glossopharyngeal nerve dysfunction. This information is crucial for developing an appropriate treatment plan tailored to the individual’s needs.
Treatment Options for Glossopharyngeal Nerve Disorders
The treatment approach for glossopharyngeal nerve disorders largely depends on the underlying cause and severity of symptoms. It is essential to consult with a healthcare professional to determine the most appropriate treatment plan.
Glossopharyngeal nerve disorders can be challenging to manage, but various treatment options are available to alleviate symptoms and improve quality of life. These treatments can range from medication therapies to surgical interventions, depending on the specific needs of the patient.
Medication Therapies
For certain glossopharyngeal nerve disorders, medication therapies may be recommended to alleviate symptoms and manage pain. These medications may include anticonvulsants, tricyclic antidepressants, or pain relievers. Anticonvulsants such as gabapentin or carbamazepine can help reduce nerve pain and prevent the occurrence of seizures. Tricyclic antidepressants like amitriptyline or nortriptyline can also be effective in managing chronic pain associated with glossopharyngeal nerve disorders. Pain relievers such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids may be prescribed for short-term relief of severe pain.
However, it is crucial to note that medication regimens should be personalized and closely monitored by healthcare professionals. The dosage and type of medication may need to be adjusted based on the individual’s response and any potential side effects. Regular follow-up appointments with the healthcare provider are necessary to ensure the effectiveness of the medication therapy.
Surgical Interventions
In cases of severe glossopharyngeal nerve dysfunction or compression, surgical interventions may be considered. These procedures aim to relieve pressure on the nerve or repair any anatomical abnormalities contributing to the dysfunction. Surgical options may include nerve decompression, microvascular decompression, or neurectomy.
Nerve decompression involves removing any structures or tissues that are compressing the glossopharyngeal nerve, such as tumors or blood vessels. Microvascular decompression is a delicate procedure that involves placing a cushioning material between the nerve and the blood vessels that may be causing compression. Neurectomy, on the other hand, involves removing a portion of the glossopharyngeal nerve itself to alleviate symptoms.
However, the decision to undergo surgery should be made after thorough discussion with healthcare specialists. The risks, benefits, and potential outcomes of the surgical intervention should be carefully considered, and the patient should be well-informed about the procedure and the recovery process.
Rehabilitation and post-operative care play a significant role in the success of surgical interventions. Physical therapy, speech therapy, and swallowing exercises may be recommended to help restore normal function and improve overall well-being.
In conclusion, the treatment options for glossopharyngeal nerve disorders are diverse and tailored to the individual’s needs. Medication therapies can provide relief from symptoms, while surgical interventions may be necessary for severe cases. The decision regarding the most appropriate treatment plan should be made in consultation with healthcare professionals, taking into consideration the underlying cause, severity of symptoms, and potential risks and benefits of each treatment option.
The Future of Glossopharyngeal Nerve Research
As medical understanding and technology advance, ongoing research offers hope for improved diagnosis and treatment of glossopharyngeal nerve disorders.
The glossopharyngeal nerve is a crucial component of the human nervous system, responsible for various functions such as taste perception, swallowing and speech coordination, and salivation stimulation. Disorders affecting this nerve, such as glossopharyngeal neuralgia or nerve damage, can significantly impact daily life.
Advances in Treatment
Ongoing research endeavors focus on identifying more effective and targeted treatments for glossopharyngeal nerve disorders. This includes exploring new medications, surgical techniques, or alternative therapeutic approaches tailored to individual needs.
One area of research involves the development of novel medications specifically designed to target glossopharyngeal nerve disorders. These medications aim to alleviate symptoms such as severe pain or difficulty swallowing, providing patients with much-needed relief and improved quality of life.
In addition to medication therapies, researchers are also investigating surgical interventions as potential treatment options. These surgical techniques aim to address the underlying causes of glossopharyngeal nerve disorders, such as nerve compression or damage. By surgically relieving pressure on the nerve or repairing damaged tissue, patients may experience significant improvements in their symptoms.
Potential for Regenerative Medicine
Regenerative medicine, a rapidly evolving field, holds promise for restoring glossopharyngeal nerve function in cases of damage or dysfunction. Researchers are exploring innovative approaches, such as stem cell therapy and tissue engineering, to regenerate or repair damaged nerves.
Stem cell therapy involves the use of specialized cells that have the potential to develop into various types of cells, including nerve cells. By introducing these cells into the damaged area of the glossopharyngeal nerve, researchers hope to stimulate the regeneration of healthy nerve tissue, restoring normal function.
Tissue engineering is another exciting avenue of research in regenerative medicine. Scientists are working on developing artificial tissues or scaffolds that can support the growth and regeneration of damaged nerves. These engineered tissues can be customized to match the specific needs of each patient, offering a personalized approach to treatment.
While these advancements in regenerative medicine are still in the experimental stages, they represent potential avenues for future treatment possibilities. Continued research and clinical trials are necessary to further explore their safety and efficacy.
In conclusion, the glossopharyngeal nerve serves several crucial functions, including taste perception, swallowing and speech coordination, and salivation stimulation. Disorders affecting this nerve, such as glossopharyngeal neuralgia or nerve damage, can significantly impact daily life. Diagnosis involves physical examination and imaging techniques, while treatment options range from medication therapies to surgical interventions.
As research in the field progresses, new advances in treatment and regenerative medicine may offer hope for individuals with glossopharyngeal nerve disorders. It is important to stay informed about the latest developments in the field and consult with healthcare professionals to determine optimal treatment options.
Remember, if you experience persistent symptoms or concerns, consult with a healthcare professional for personalized guidance and care.