The glossopharyngeal nerve is an important cranial nerve that plays a crucial role in several vital functions of the human body. Testing the glossopharyngeal nerve can provide valuable insights into a patient’s overall health and help diagnose potential underlying conditions. In this article, we will explore the process of testing the glossopharyngeal nerve, including its anatomy, functions, necessary equipment, step-by-step procedure, interpreting the test results, potential complications, and post-test care.
Understanding the Glossopharyngeal Nerve
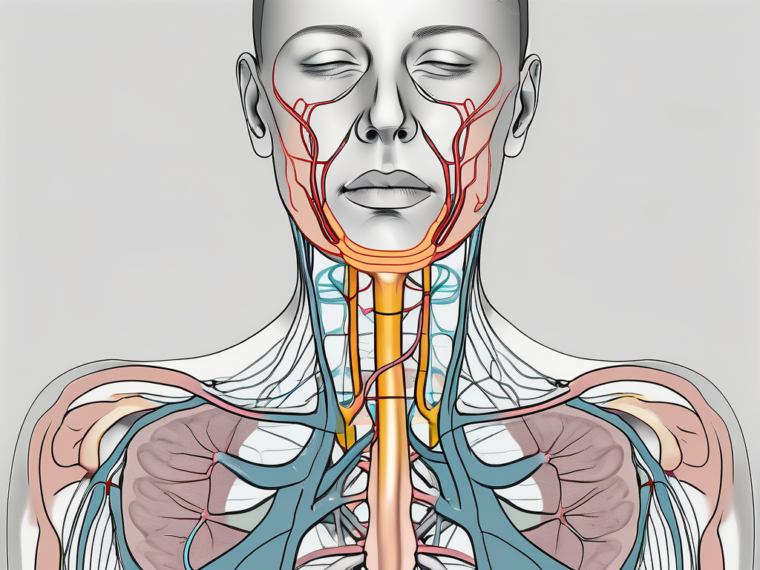
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves originating from the brain. It is primarily responsible for transmitting sensory and motor signals to and from the throat, tongue, and certain regions of the ear.
The glossopharyngeal nerve plays a crucial role in the overall functioning of the head and neck region. It is involved in various important processes, such as swallowing, taste perception, and providing sensory information from the throat and middle ear.
Anatomy of the Glossopharyngeal Nerve
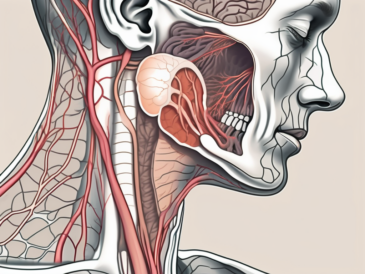
The glossopharyngeal nerve arises from the medulla oblongata, a region located at the base of the brainstem. It consists of both sensory and motor fibers, which carry different types of information to and from various parts of the body.
The sensory fibers of the glossopharyngeal nerve provide sensation to the back of the throat, tonsils, middle ear, and the posterior one-third of the tongue. These sensory signals play a crucial role in our ability to taste, swallow, and perceive sensations in these areas.
Additionally, the glossopharyngeal nerve contributes to taste perception in certain areas of the tongue. It carries taste signals from taste buds located in the posterior one-third of the tongue to the brain, allowing us to savor and differentiate various flavors.
On the other hand, the motor fibers of the glossopharyngeal nerve control the muscles involved in swallowing and elevating the pharynx during eating and talking. These motor signals ensure the smooth and coordinated movement of the throat muscles, facilitating the process of swallowing and preventing food or liquid from entering the airway.
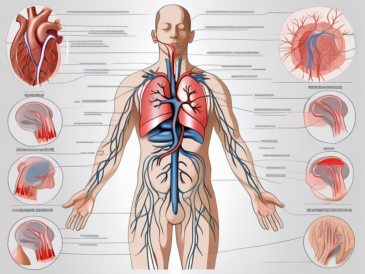
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve serves several important functions, including:
- Mediating the sensation of taste in the posterior one-third of the tongue: The glossopharyngeal nerve plays a crucial role in our ability to taste and appreciate different flavors. It carries taste signals from the taste buds located in the posterior one-third of the tongue to the brain, allowing us to enjoy the diverse range of tastes.
- Providing sensory information from the throat, tonsils, and middle ear: The glossopharyngeal nerve acts as a sensory pathway, transmitting important information from the throat, tonsils, and middle ear to the brain. This sensory input helps us perceive sensations, such as pain, temperature, and pressure, in these regions.
- Controlling muscles involved in swallowing and throat movements: The motor fibers of the glossopharyngeal nerve are responsible for controlling the muscles involved in swallowing and throat movements. These muscles work together to facilitate the smooth passage of food and liquid through the throat, ensuring efficient digestion and preventing choking.
Now that we have gained a better understanding of the glossopharyngeal nerve, let’s delve into the process of testing this vital cranial nerve.
Preparing for the Glossopharyngeal Nerve Test
Before conducting the glossopharyngeal nerve test, it is essential to gather the necessary equipment and ensure that the patient is adequately prepared.
The glossopharyngeal nerve test is a diagnostic procedure used to assess the function of the glossopharyngeal nerve, which is responsible for various vital functions in the throat and tongue. This test helps healthcare professionals identify any abnormalities or impairments in the nerve’s function, allowing for appropriate treatment and management.
Necessary Equipment for the Test
To perform the glossopharyngeal nerve test, the following equipment is typically required:
- Tongue depressor: A tongue depressor is a flat, thin instrument used to hold down the tongue during the examination. It allows for a clear view of the throat and facilitates the assessment of the patient’s gag reflex.
- Flashlight: A flashlight is used to provide adequate lighting during the examination. It helps illuminate the oral cavity, making it easier to observe any abnormalities or changes in the throat.
- Gauze or cotton swabs: Gauze or cotton swabs are used to gently clean the area being examined, ensuring a clear view of the throat and preventing any interference with the test results.
- Thermometer: A thermometer may be used to measure the patient’s temperature, as certain conditions affecting the glossopharyngeal nerve can cause fluctuations in body temperature.
These tools aid in examining the throat, assessing the patient’s gag reflex, and potentially identifying any abnormalities in the glossopharyngeal nerve function.
Patient Preparation Guidelines
Prior to the test, it is crucial to provide the patient with clear instructions and ensure their comfort. Here are some general patient preparation guidelines:
- Inform the patient about the purpose of the test and its potential benefits. This helps alleviate any anxiety or concerns they may have and ensures their cooperation throughout the procedure.
- Explain the procedure in detail, addressing any concerns or questions they may have. It is essential to provide a step-by-step explanation, ensuring that the patient understands what to expect during the test.
- Obtain informed consent from the patient, ensuring they understand the nature of the test and its potential outcomes. Informed consent involves explaining the risks, benefits, and alternatives of the procedure, allowing the patient to make an informed decision.
- Advise the patient to refrain from eating or drinking for a specific period before the test, as instructed by their healthcare provider. This fasting period ensures that the test results are not affected by recent food or beverage consumption.
- Ensure an appropriate clinical setting with adequate lighting and a comfortable examination table or chair. A well-lit and comfortable environment helps the patient relax and allows the healthcare professional to perform the test more effectively.
By following these patient preparation guidelines, healthcare professionals can create a conducive environment for accurate glossopharyngeal nerve testing. Adequate preparation ensures that the test results are reliable and helps healthcare providers make informed decisions regarding the patient’s diagnosis and treatment plan.
Step-by-Step Procedure of the Glossopharyngeal Nerve Test
The glossopharyngeal nerve test involves a systematic assessment of various aspects related to throat function and sensory perception. The following step-by-step procedure outlines the main components of the test:
Initial Assessment
The healthcare professional begins by conducting a comprehensive assessment of the patient’s medical history, including any past or existing conditions that may affect the glossopharyngeal nerve. This initial evaluation helps the examiner understand the patient’s specific needs and tailor the test accordingly.
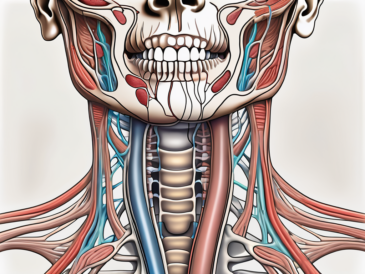
Once the medical history has been reviewed, a physical examination of the patient’s throat and mouth is performed. Visual inspection and palpation techniques are utilized to identify any abnormalities, swelling, or tenderness that could indicate issues with the glossopharyngeal nerve.
During the physical examination, the healthcare professional may use a small light source to illuminate the oral cavity, allowing for a more detailed examination. This can help identify any lesions, ulcers, or other abnormalities that may be affecting the glossopharyngeal nerve function.
Furthermore, the healthcare professional may also perform a cranial nerve examination to assess the overall function of the patient’s cranial nerves, including the glossopharyngeal nerve. This examination involves various tests to evaluate the patient’s ability to perform specific movements and perceive sensory stimuli.
Performing the Test
After the initial assessment, the actual glossopharyngeal nerve test is executed. The healthcare professional follows these steps:
- Using a tongue depressor, the examiner assesses the patient’s gag reflex by gently touching the back of the throat. The absence or presence of the gag reflex provides valuable insights into the glossopharyngeal nerve function.
- A flashlight is employed to visually examine the tonsils, throat, and posterior one-third of the tongue. Any abnormalities, such as asymmetry or swelling, should be carefully noted.
- Gauze or cotton swabs may be used to apply gentle pressure to specific areas of the throat or tongue. The patient is instructed to report any sensations or discomfort experienced during this process.
- To evaluate temperature sensation, a thermometer or a specialized thermal device may be employed. The patient will be asked to indicate whether they perceive warm or cold sensations on their throat or tongue.
The healthcare professional may also ask the patient to swallow during the examination to further evaluate the glossopharyngeal nerve’s role in coordinating swallowing movements and preventing aspiration.
In addition to visual examination, the healthcare professional may use a tongue depressor or a spatula to gently lift the tongue and inspect the base of the tongue and the area near the tonsils. This allows for a more thorough assessment of the glossopharyngeal nerve’s sensory function in these regions.
The healthcare professional may also use a cotton swab soaked in a taste solution to assess the patient’s ability to taste different flavors. This can provide additional information about the glossopharyngeal nerve’s role in gustatory sensation.
In some cases, the healthcare professional may also use a tuning fork or other vibrating device to assess the patient’s ability to perceive vibration in the throat or tongue. This test can provide insights into the glossopharyngeal nerve’s role in proprioception and vibration sensation.
The above steps constitute the key components of the glossopharyngeal nerve test. However, additional assessments or procedures may be necessary based on the individual patient’s condition and the healthcare provider’s clinical judgment.
Interpreting the Test Results
Upon completing the glossopharyngeal nerve test, the healthcare professional evaluates the results to determine the functioning of the glossopharyngeal nerve. The interpretation of test findings is crucial in identifying potential abnormalities or underlying health conditions.
The glossopharyngeal nerve test is a diagnostic procedure used to assess the functionality of the glossopharyngeal nerve, which is responsible for various important functions in the throat and tongue. This nerve plays a key role in the gag reflex, as well as in the perception of temperature and pressure in specific areas of the mouth and throat.
Normal Findings
In ideal circumstances, a glossopharyngeal nerve test would yield normal findings, indicating that the nerve is functioning within normal parameters. This implies that the patient’s gag reflex is intact, the throat and tongue appear healthy, and the sensory perception of temperature and pressure in the relevant areas is appropriate.
A normal glossopharyngeal nerve test result provides reassurance to both the healthcare professional and the patient, as it suggests that there are no significant abnormalities or underlying health conditions affecting the glossopharyngeal nerve. This can help rule out certain conditions and provide valuable information for further medical management.
Abnormal Findings
Abnormal findings from the glossopharyngeal nerve test may suggest various issues, including but not limited to:
- Glossopharyngeal neuralgia: This condition is characterized by severe pain in the throat, tongue, and ear, often triggered by swallowing or speaking. It can be caused by irritation or damage to the glossopharyngeal nerve.
- Tumors or growths affecting the nerve: Abnormal growths in the throat or surrounding areas can put pressure on the glossopharyngeal nerve, leading to dysfunction and abnormal test results.
- Inflammation or infection in the tonsils or throat: Conditions such as tonsillitis or pharyngitis can cause inflammation or infection in the throat, potentially affecting the glossopharyngeal nerve and its function.
- Nerve damage or dysfunction: Trauma, certain medical conditions, or underlying neurological disorders can result in damage or dysfunction of the glossopharyngeal nerve, leading to abnormal test findings.
If abnormal findings are identified during the glossopharyngeal nerve test, further diagnostic investigations may be necessary to determine the cause and appropriate management plan. The healthcare professional may recommend additional tests, such as imaging studies or nerve conduction studies, to gather more information and accurately diagnose the underlying condition.
It is crucial for the patient to consult with a healthcare professional for accurate diagnosis and treatment options. The healthcare professional will consider the test results, medical history, and other relevant factors to develop an individualized treatment plan tailored to the patient’s specific needs. Prompt diagnosis and appropriate management can help alleviate symptoms, improve overall health, and prevent potential complications associated with glossopharyngeal nerve dysfunction.
Potential Complications and Risks
While the glossopharyngeal nerve test is generally regarded as safe and non-invasive, there are potential complications and risks associated with the procedure that healthcare professionals should be aware of.
Risks Associated with the Test
The risks associated with the glossopharyngeal nerve test are minimal, but they may include:
- Discomfort or minor pain during the examination
- Temporary gagging or retching in sensitive individuals
- Rare cases of bleeding or infection, particularly if an invasive procedure is necessary
Healthcare providers should exercise caution and follow appropriate guidelines to minimize these risks and ensure patient safety.
How to Manage Potential Complications
If complications arise during or after a glossopharyngeal nerve test, healthcare professionals should take the necessary steps to manage them effectively. This may include:
- Providing reassurance and comfort to the patient
- Administering appropriate pain relief or topical anesthesia, if required
- Addressing any bleeding or signs of infection with proper wound care techniques
If complications persist or worsen, it is crucial to promptly involve a healthcare professional to determine the best course of action.
Post-Test Care and Follow-up
After the completion of the glossopharyngeal nerve test, certain post-test care measures should be implemented to ensure the patient’s well-being and facilitate recovery.
Immediate Post-Test Care
Following the test, it is advisable to provide the patient with the following instructions:
- Allow some time for the patient to rest and recover, especially if they experienced any discomfort or stress during the test.
- Encourage the patient to resume their regular activities, unless advised otherwise by their healthcare provider.
- Discuss any immediate findings or concerns with the patient, explaining the potential implications and advising them on the next steps.
If necessary, healthcare professionals may offer additional guidance specific to the patient’s condition or the purpose of the glossopharyngeal nerve test.
Long-Term Follow-up and Management
Long-term follow-up and management are crucial aspects of patient care, especially for individuals who have received abnormal findings during the glossopharyngeal nerve test or have been diagnosed with an associated condition.
Healthcare professionals should:
- Coordinate appropriate referrals to specialists for further evaluation and treatment, if required.
- Communicate test results and relevant information to the patient’s primary healthcare provider, ensuring continuity of care.
- Schedule regular follow-up appointments to monitor the patient’s progress, assess treatment effectiveness, and address any emerging concerns.
By prioritizing long-term follow-up and management, healthcare professionals can play a crucial role in promoting the patient’s well-being and achieving optimal health outcomes.
Frequently Asked Questions about Glossopharyngeal Nerve Test
Here are the answers to some frequently asked questions related to the glossopharyngeal nerve test:
What to Expect During the Test?
During the glossopharyngeal nerve test, patients can expect a thorough examination of their throat, tonsils, and tongue. The healthcare professional may employ tools like a tongue depressor, flashlight, or thermal device to assess the patient’s throat function and sensory perception. Although the test may cause occasional discomfort or gagging sensations, it is generally well-tolerated and non-invasive.
How Long Does the Test Take?
The duration of the glossopharyngeal nerve test can vary depending on various factors, such as the patient’s condition, the complexity of the examination, and additional investigations required. On average, the test itself usually takes between 10 to 30 minutes. However, it is important to note that the entire process, including patient preparation and post-test care, may require additional time.
In conclusion, testing the glossopharyngeal nerve is a valuable diagnostic tool that can provide crucial insights into a patient’s overall health and help identify potential issues. Healthcare professionals should follow the appropriate guidelines, utilize the necessary equipment, and interpret the test results accurately. It is important to remember that while this article provides an overview of the glossopharyngeal nerve test, individuals should always consult with a healthcare professional for personalized advice and guidance tailored to their specific needs.