The glossopharyngeal nerve plays a crucial role in various functions related to swallowing and sensation in the oropharynx. Assessing its function can provide valuable insights into certain medical conditions. This article aims to provide an overview of how to quickly test glossopharyngeal nerve function, including understanding the nerve’s anatomy, preparing for the test, implementing the step-by-step procedure, interpreting test results, and addressing safety measures and precautions. Please note that this article does not provide medical advice, and it is important to consult with a healthcare professional for diagnosis and treatment.
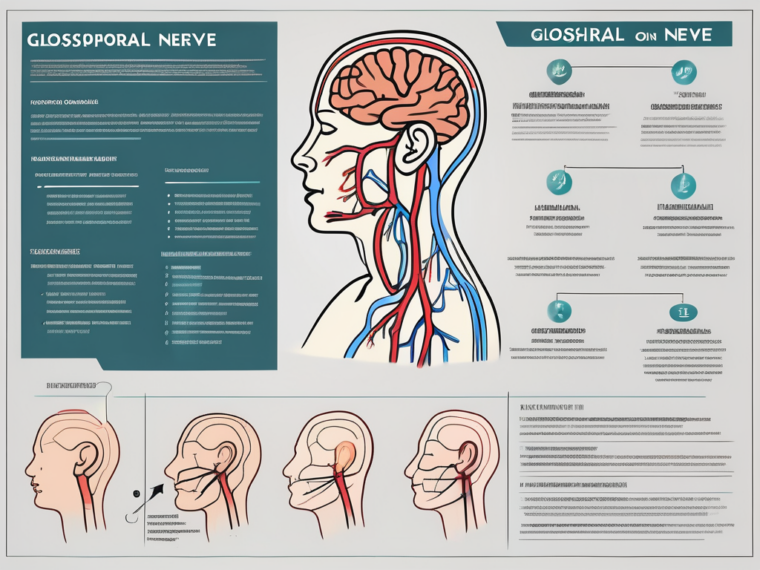
Understanding the Glossopharyngeal Nerve
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves. It originates in the medulla oblongata, a vital part of the brainstem responsible for controlling various autonomic functions, and travels down to the throat, branching out to various structures in the oropharynx region.
Comprised of both sensory and motor fibers, the glossopharyngeal nerve plays a vital role in swallowing, taste sensation, and monitoring blood pressure. Let’s explore the intricate anatomy and fascinating functions of this remarkable nerve.
Anatomy of the Glossopharyngeal Nerve
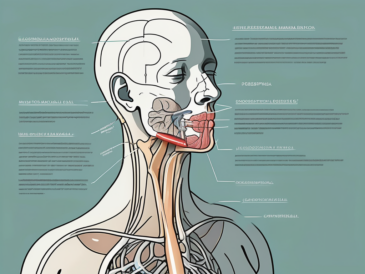
The glossopharyngeal nerve has complex anatomy, with connections to the medulla oblongata and various structures in the oral cavity, throat, and neck. It arises from multiple origins, including the posterior aspect of the medulla oblongata and the upper spinal cord levels. From its origins, the nerve descends through the skull and neck, passing through the jugular foramen, a narrow opening at the base of the skull.
As it continues its journey, the glossopharyngeal nerve branches out to innervate several important structures. It sends sensory fibers to the posterior third of the tongue, providing taste sensation and general sensory information. Additionally, it receives sensory input from the pharynx, tonsils, middle ear, and the carotid sinus, which is a specialized area in the carotid artery responsible for monitoring blood pressure.
Motor fibers from the glossopharyngeal nerve innervate muscles involved in swallowing and speech. These motor branches control the stylopharyngeus muscle, which helps elevate the pharynx during swallowing and plays a role in the production of speech sounds.
Role and Function of the Glossopharyngeal Nerve
The glossopharyngeal nerve serves several key functions related to taste sensation, swallowing, and blood pressure regulation. It carries sensory information from the posterior third of the tongue, along with taste buds on the tongue’s base. This allows us to perceive the different tastes of food and beverages, enhancing our overall sensory experience.
In addition to taste sensation, the glossopharyngeal nerve plays a crucial role in the gag reflex, which is a protective mechanism that helps prevent choking. When an object or substance touches the back of the throat, the nerve triggers the contraction of certain muscles, including the stylopharyngeus muscle, to initiate the swallowing reflex and clear the airway.
Furthermore, the glossopharyngeal nerve is involved in monitoring blood pressure through its connection to the carotid sinus. Changes in blood pressure are detected by specialized receptors in the carotid sinus, and this information is transmitted through the glossopharyngeal nerve to the brainstem. This feedback loop allows the body to maintain blood pressure within a normal range and respond appropriately to changes in physiological conditions.
In conclusion, the glossopharyngeal nerve is a remarkable cranial nerve with a complex anatomy and diverse functions. From its origins in the medulla oblongata to its innervation of various structures in the oral cavity, throat, and neck, this nerve plays a vital role in taste sensation, swallowing, and blood pressure regulation. Its intricate connections and functions highlight the intricate nature of the human nervous system and its ability to coordinate essential bodily processes.
Preparing for the Glossopharyngeal Nerve Test
Prior to conducting the glossopharyngeal nerve test, healthcare professionals must ensure they have the necessary equipment and adhere to patient preparation guidelines.
Necessary Equipment for the Test
The glossopharyngeal nerve test requires specific equipment, including a tongue depressor, a cotton swab or applicator stick for performing the taste test, and a penlight or flashlight for visual examination of the throat.
When it comes to the tongue depressor, it is typically made of wood or plastic and is used to hold down the tongue during the examination. This allows healthcare professionals to have a clear view of the throat and the glossopharyngeal nerve. The cotton swab or applicator stick is used to apply different tastes to the back of the patient’s tongue, testing their ability to perceive different flavors. Lastly, the penlight or flashlight is used to illuminate the throat, aiding in the visual examination of the glossopharyngeal nerve.
Patient Preparation Guidelines
Proper patient preparation is essential to ensure accurate test results. Informing the patient about the procedure is crucial in establishing trust and cooperation. Healthcare professionals should explain the purpose of the test, which is to assess the function of the glossopharyngeal nerve, as well as the expected duration of the examination. It is important to note that while the test may cause some discomfort, it is generally well-tolerated by patients.
One important aspect of patient preparation is instructing the patient to refrain from eating or drinking for a specified period before the test. This is because taste perception can be influenced by recent consumption of food or beverages. By ensuring that the patient has an empty stomach, healthcare professionals can obtain more accurate results during the taste test portion of the examination.
Furthermore, healthcare professionals should gather information about the patient’s medications and medical conditions that could potentially impact the test results. Certain medications, such as those affecting taste perception or the gag reflex, may need to be temporarily discontinued or adjusted prior to the test. Additionally, medical conditions that can affect the function of the glossopharyngeal nerve, such as neurological disorders or throat infections, should be taken into consideration during patient preparation.
Overall, proper patient preparation and the use of necessary equipment are crucial in ensuring the accuracy and effectiveness of the glossopharyngeal nerve test. By following these guidelines, healthcare professionals can confidently assess the function of the glossopharyngeal nerve and provide appropriate care and treatment based on the test results.
Step-by-Step Procedure for Testing Glossopharyngeal Nerve Function
The glossopharyngeal nerve function test involves a series of assessments and examinations to evaluate the nerve’s integrity and responsiveness.
Initial Assessment
Before commencing the specific tests, begin by conducting an initial assessment of the patient. This may involve taking a detailed medical history and performing a physical examination to identify any potential underlying issues that could affect the glossopharyngeal nerve function.
During the medical history, inquire about any previous medical conditions or surgeries that may have impacted the glossopharyngeal nerve. Pay attention to symptoms such as difficulty swallowing, changes in taste perception, or any other relevant complaints that could indicate glossopharyngeal nerve dysfunction.
During the physical examination, assess the patient’s general appearance, looking for any signs of facial asymmetry or muscle weakness that could be associated with glossopharyngeal nerve impairment. Additionally, evaluate the patient’s ability to swallow by observing their swallowing reflex and noting any abnormalities or difficulties.
Performing the Gag Reflex Test
The gag reflex test assesses the glossopharyngeal nerve’s role in the reflexive contraction of certain throat muscles. To perform this test, gently touch the back of the patient’s throat with a tongue depressor. Observe the patient’s reaction and note any signs of a normal or abnormal gag reflex.
A normal gag reflex involves the contraction of the muscles at the back of the throat, while an abnormal gag reflex may be absent or reduced. Document any variations in the strength or absence of the gag reflex, as it can provide valuable information about the glossopharyngeal nerve’s function.
It is important to note that the gag reflex can be influenced by factors other than glossopharyngeal nerve dysfunction, such as anxiety or previous traumatic experiences. Therefore, it should be interpreted in conjunction with other tests and clinical findings.
Conducting the Taste Test
To evaluate the glossopharyngeal nerve’s involvement in taste sensation, apply a small amount of taste stimulus, such as a sugar solution or bitter substance, to the posterior third of the patient’s tongue using a cotton swab or applicator stick. Monitor the patient’s response and record any abnormalities in their ability to perceive taste.
The glossopharyngeal nerve carries taste information from the posterior third of the tongue, so any dysfunction in this nerve can result in altered taste perception. During the taste test, ask the patient to identify the taste they perceive and compare it to the expected response. Document any discrepancies or abnormalities in taste perception.
It is important to consider that taste perception can be influenced by factors other than glossopharyngeal nerve dysfunction, such as nasal congestion or medication side effects. Therefore, it is crucial to rule out these factors and interpret the test results in the context of the patient’s overall clinical presentation.
Interpreting the Test Results
Interpretation of the glossopharyngeal nerve test results requires knowledge of the normal versus abnormal responses and an understanding of potential disorders associated with glossopharyngeal nerve dysfunction.
The glossopharyngeal nerve test is a crucial diagnostic tool used to assess the function of the glossopharyngeal nerve, which plays a vital role in swallowing, taste perception, and the gag reflex. By evaluating the responses elicited during this test, healthcare professionals can gather valuable information about the integrity of the glossopharyngeal nerve and identify any potential abnormalities or dysfunctions.
Normal vs Abnormal Results
A normal gag reflex and accurate taste perception indicate proper glossopharyngeal nerve function. When the glossopharyngeal nerve is functioning optimally, the gag reflex is triggered appropriately, protecting the airway from potential foreign objects or substances. Additionally, accurate taste perception allows individuals to savor the flavors of different foods and beverages.
On the other hand, abnormalities in the glossopharyngeal nerve test results may suggest nerve damage or dysfunction. Reduced or absent reflex response during the gag reflex test may indicate impaired glossopharyngeal nerve function. Altered taste perception, such as an inability to detect certain tastes or experiencing unusual taste sensations, can also be indicative of glossopharyngeal nerve dysfunction.
It is important to note that abnormal test results do not provide a definitive diagnosis but rather serve as an indication that further investigation is needed. Additional tests and evaluations may be required to determine the underlying cause of the glossopharyngeal nerve dysfunction.
Potential Disorders Related to Glossopharyngeal Nerve Dysfunction
Glossopharyngeal nerve dysfunction can occur due to various medical conditions, each with its own set of symptoms and implications. One such condition is glossopharyngeal neuralgia, a rare but debilitating disorder characterized by severe pain in the throat, tonsillar region, or base of the tongue. This excruciating pain can be triggered by activities such as swallowing, speaking, or even touching the affected areas.
Infections can also affect the function of the glossopharyngeal nerve. Conditions like tonsillitis, pharyngitis, or even systemic infections can lead to inflammation and subsequent nerve dysfunction. Similarly, tumors in the vicinity of the glossopharyngeal nerve can exert pressure on the nerve fibers, causing impairment in its function.
Trauma to the cranial nerves, including the glossopharyngeal nerve, can result from accidents, head injuries, or surgical procedures. Any damage to the nerve can disrupt its normal functioning and lead to various symptoms, depending on the extent and location of the injury.
It is essential for healthcare professionals to consider these potential disorders when interpreting glossopharyngeal nerve test results. By understanding the underlying conditions associated with glossopharyngeal nerve dysfunction, appropriate treatment plans can be developed to address the specific needs of each individual patient.
Safety Measures and Precautions
When conducting the glossopharyngeal nerve test, it is crucial to take certain safety measures and precautions to minimize risks and ensure the well-being of the patient.
One important safety measure is to ensure that the healthcare professional performing the test is well-trained and experienced in this specific procedure. This will help minimize the chances of any errors or complications during the test.
Additionally, it is essential to have the necessary equipment and tools readily available and in good working condition. This includes ensuring that the instruments used for the test are properly sterilized to prevent any potential infections or cross-contamination.
Furthermore, it is important to obtain informed consent from the patient before conducting the glossopharyngeal nerve test. This involves explaining the purpose of the test, the potential risks and benefits, and any alternative options available. This ensures that the patient is fully aware of what to expect and can make an informed decision regarding their participation in the test.
Risks and Complications of the Test
The glossopharyngeal nerve test, when performed appropriately, carries minimal risk. However, some patients may experience temporary discomfort or gagging during the procedure. Healthcare professionals must be attentive and responsive to any adverse reactions and address them promptly.
In rare cases, there may be a risk of injury to the glossopharyngeal nerve or surrounding structures. This can occur if the test is not performed correctly or if there are anatomical variations in the patient’s anatomy. To minimize this risk, healthcare professionals should exercise caution and carefully follow established guidelines and protocols.
It is also important to note that certain medical conditions or medications may increase the risk of complications during the glossopharyngeal nerve test. For example, patients with bleeding disorders or those taking blood-thinning medications may be more prone to bleeding or bruising at the site of the test. Healthcare professionals should take these factors into consideration and assess the patient’s medical history before proceeding with the test.
Post-Test Care and Management
After completing the glossopharyngeal nerve test, provide appropriate post-test care instructions to the patient. This may include advice on resuming normal activities and addressing any concerns or complications that may arise following the procedure.
Patients should be advised to monitor for any signs of infection, such as increased pain, redness, swelling, or discharge at the site of the test. If any of these symptoms occur, they should seek medical attention promptly.
Furthermore, patients should be informed about the importance of following up with their healthcare provider to discuss the test results. Depending on the findings, further evaluation or management strategies may be necessary. It is crucial for patients to understand the significance of these results and the potential implications for their overall health and well-being.
Encourage patients to ask any questions or voice any concerns they may have regarding the test or its results. Providing them with the necessary support and information can help alleviate anxiety and ensure their continued engagement in their healthcare journey.
Frequently Asked Questions about Glossopharyngeal Nerve Testing
It is natural for patients to have questions regarding the glossopharyngeal nerve test. Here are some commonly asked questions along with brief answers.
What to Expect During the Test?
The glossopharyngeal nerve test involves a series of assessments, including the evaluation of the gag reflex and taste perception. It is usually a quick and straightforward procedure that can provide valuable information about the functioning of the glossopharyngeal nerve.
How Long Does the Test Take?
The duration of the glossopharyngeal nerve test can vary depending on individual factors and the complexity of the case. Generally, the test can be completed within a few minutes, and results can be obtained promptly.
When to Seek Medical Help After the Test?
If patients experience any unexpected symptoms, complications, or concerns following the glossopharyngeal nerve test, they should seek immediate medical attention. It is important not to ignore any issues and consult with a healthcare professional for appropriate evaluation and guidance.
In conclusion, understanding how to quickly test glossopharyngeal nerve function can provide valuable insights into various medical conditions. By following the step-by-step procedure, healthcare professionals can assess the nerve’s integrity and responsiveness. However, it is important to note that this article does not provide medical advice, and it is essential to consult with a healthcare professional for a comprehensive evaluation and appropriate management strategies.