The glossopharyngeal nerve is a crucial nerve responsible for various functions in the human body. In this article, we will delve into the intricacies of palpating the glossopharyngeal nerve and provide valuable insights on its anatomy, function, and interpretation of palpation results. Furthermore, we will discuss necessary equipment, safety measures, and post-palpation procedures to ensure a comprehensive understanding of this diagnostic technique.
Understanding the Glossopharyngeal Nerve
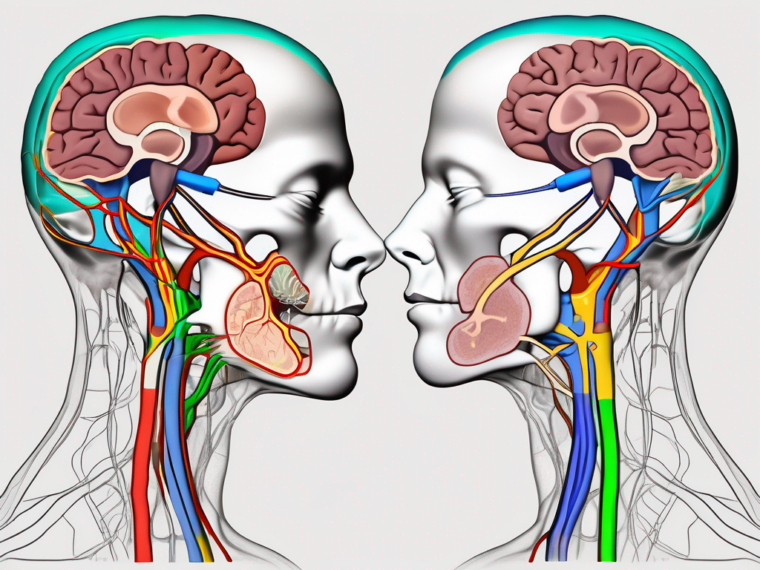
The glossopharyngeal nerve, also known as the ninth cranial nerve, originates from the medulla oblongata within the brainstem. It consists of both sensory and motor fibers, enabling it to serve multiple functions.
The sensory fibers of the glossopharyngeal nerve are responsible for transmitting sensations from the tongue, throat, and other structures within the oral cavity. These sensory inputs play a crucial role in taste perception, touch sensitivity, and the gag reflex.
On the other hand, the motor fibers of the glossopharyngeal nerve innervate certain muscles involved in swallowing and speech production.
Anatomy of the Glossopharyngeal Nerve
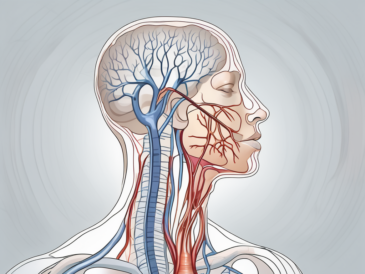
The glossopharyngeal nerve is a complex structure that extends from the medulla oblongata to various regions within the oral cavity. It consists of multiple branches that innervate specific areas, allowing for precise control and coordination.
One of the main branches of the glossopharyngeal nerve is the lingual branch, which supplies sensory fibers to the posterior third of the tongue. These fibers are responsible for transmitting taste signals from the taste buds located in this region.
Another important branch is the pharyngeal branch, which innervates the muscles involved in swallowing. These muscles work together to propel food from the mouth to the esophagus, ensuring efficient digestion.
Furthermore, the glossopharyngeal nerve gives rise to the tympanic branch, which plays a role in transmitting sensory information from the middle ear. This branch is involved in the regulation of hearing and balance, contributing to our overall perception of sound and spatial orientation.
Function of the Glossopharyngeal Nerve
The glossopharyngeal nerve performs a wide array of functions. Its sensory component enables taste perception, transmitting signals from the taste buds located on the posterior third of the tongue. This allows us to experience the diverse flavors of the foods we consume, enhancing our enjoyment of meals.
Furthermore, the glossopharyngeal nerve carries tactile information from the tongue, throat, and tonsils. This sensory input helps us distinguish between different textures and temperatures, allowing us to savor the variety of sensations that come with eating and drinking.
In addition to its role in taste and touch, the glossopharyngeal nerve is also involved in regulating blood pressure. It does so by monitoring carotid sinus baroreceptors, which are specialized sensors located in the carotid arteries. These receptors detect changes in blood pressure and send signals to the brain, triggering appropriate adjustments to maintain cardiovascular homeostasis.
Moreover, the glossopharyngeal nerve communicates information from the carotid body, another structure located in the carotid arteries. The carotid body is responsible for monitoring changes in blood oxygen and carbon dioxide levels. By relaying this information to the brain, the glossopharyngeal nerve helps maintain the body’s respiratory function and overall metabolic balance.
Additionally, the glossopharyngeal nerve is involved in the gag reflex, a protective mechanism that prevents foreign objects from entering the airway. When stimulated, this reflex triggers a series of muscular contractions in the throat, expelling any potential threats and ensuring the safety of the respiratory system.
Dysfunction of the glossopharyngeal nerve can lead to issues with swallowing, speech, and taste perception. Conditions such as glossopharyngeal neuralgia, where the nerve becomes irritated or compressed, can cause severe pain in the throat, tongue, and ear. Proper understanding of the anatomy and function of the glossopharyngeal nerve is crucial for diagnosing and treating such conditions effectively.
Preparing for the Palpation Procedure
Palpating the glossopharyngeal nerve requires careful preparation to ensure accuracy and patient safety. In addition to having a thorough understanding of the procedure, it is important to gather the necessary equipment and take appropriate safety measures.
Necessary Equipment for Palpation
Before embarking on the journey of palpating the glossopharyngeal nerve, it is imperative to gather the necessary equipment. This includes disposable gloves, a good source of lighting, and a tongue depressor for facilitating access to the oral cavity.
Disposable gloves are essential to maintain a sterile environment and prevent the transmission of pathogens. They provide a barrier between the healthcare provider’s hands and the patient’s oral cavity, reducing the risk of contamination.
A good source of lighting is crucial for visualizing the oral cavity and ensuring accurate palpation. It allows for better visibility of the structures involved, making it easier to locate and palpate the glossopharyngeal nerve.
The tongue depressor plays a vital role in facilitating access to the oral cavity. By depressing the tongue, it provides a clear view of the structures in the posterior part of the mouth, making it easier to identify and palpate the glossopharyngeal nerve.
It is crucial to ensure that all equipment is sterile and in proper working condition to minimize the risk of infection or inaccuracies in the palpation procedure. Regular maintenance and inspection of the equipment are necessary to guarantee their effectiveness.
Safety Measures and Precautions
Prior to palpation, it is essential to adhere to safety measures to ensure patient comfort and prevent any potential complications. Firstly, obtaining informed consent from the patient is crucial, allowing them to understand and consent to the procedure. This ensures that the patient is fully aware of the purpose, potential risks, and benefits of the palpation.
It is essential to maintain strict aseptic technique throughout the procedure to minimize the risk of infection. This includes proper hand hygiene, implementing sterile gloves, and ensuring the cleanliness of all materials used. Hand hygiene should be performed using soap and water or an alcohol-based hand sanitizer, following the recommended guidelines for duration and technique.
Additionally, it is important to create a comfortable and safe environment for the patient during the palpation procedure. This includes ensuring privacy, providing clear instructions, and addressing any concerns or questions they may have. Patient comfort and trust are essential for a successful and effective palpation.
Furthermore, healthcare providers should be aware of any contraindications or precautions related to the palpation procedure. This includes assessing the patient’s medical history, allergies, and any potential risks that may affect the procedure. By identifying and addressing these factors, healthcare providers can ensure the safety and well-being of the patient.
In conclusion, preparing for the palpation of the glossopharyngeal nerve involves gathering the necessary equipment, ensuring their sterility and functionality, and taking appropriate safety measures. By following these steps, healthcare providers can conduct a successful and safe palpation procedure, providing valuable information for diagnosis and treatment planning.
Steps to Palpate the Glossopharyngeal Nerve
Locating the Glossopharyngeal Nerve
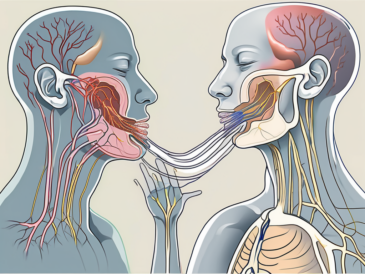
The glossopharyngeal nerve can be challenging to locate due to its intricate anatomical pathway. To facilitate accurate palpation, the patient is typically positioned comfortably in an upright or supine position, with proper lighting for adequate visualization.
The glossopharyngeal nerve can be palpated manually by gently exploring the posterior third of the tongue and the soft palate. Careful and precise palpation is essential to avoid causing discomfort or injury to the patient.
As the practitioner begins the palpation process, it is important to note that the glossopharyngeal nerve is one of the cranial nerves responsible for various functions, including taste sensation, swallowing, and the gag reflex. By palpating this nerve, healthcare professionals can assess its functionality and detect any abnormalities that may be present.
Moreover, understanding the anatomical landmarks surrounding the glossopharyngeal nerve is crucial for successful palpation. The practitioner must be familiar with the location of the tonsils, the base of the tongue, and the uvula, as these structures can serve as reference points during the examination.
Techniques for Effective Palpation
When palpating the glossopharyngeal nerve, it is vital to employ gentle and controlled movements to ensure accurate assessment without causing unnecessary discomfort. Using a tongue depressor, the practitioner can enhance visualization and access to the deep structures of the oral cavity.
During the palpation process, the healthcare professional may also utilize other techniques to enhance the examination. For instance, the practitioner may ask the patient to perform specific actions, such as swallowing or sticking out their tongue, to further evaluate the glossopharyngeal nerve’s functionality.
Communication with the patient throughout the palpation procedure is crucial. Explaining each step and reassuring the patient can help alleviate any anxiety or fear they may experience during the process.
Furthermore, it is important to consider the patient’s medical history and any underlying conditions that may affect the glossopharyngeal nerve’s function. Conditions such as glossopharyngeal neuralgia, tumors, or infections can impact the nerve’s sensitivity and response to palpation.
By employing a comprehensive approach to palpating the glossopharyngeal nerve, healthcare professionals can gather valuable information about the patient’s overall health and identify any potential issues that may require further investigation or treatment.
Interpreting Palpation Results
When it comes to interpreting the results of glossopharyngeal nerve palpation, a comprehensive understanding of the normal anatomy and expected variations is crucial. In a healthy individual, the glossopharyngeal nerve should exhibit an adequate response to palpation, indicating proper functioning.
However, it is important to keep in mind that anatomical variations may exist between individuals. Each person’s anatomy is unique, and this can influence the palpation results. Therefore, when interpreting palpation findings, it is essential to consider the patient’s specific characteristics and anatomical variations.
Normal Findings and Variations
Understanding the normal findings and variations of the glossopharyngeal nerve is essential for accurate interpretation. The glossopharyngeal nerve is responsible for various functions, including taste perception, swallowing, and the sensation of the posterior third of the tongue, tonsils, and pharynx.
In a healthy individual, the glossopharyngeal nerve should exhibit normal responses to palpation. This means that the patient should not experience any discomfort or abnormal sensations during the palpation process. Additionally, the muscles innervated by the glossopharyngeal nerve should demonstrate proper motor function.
However, it is important to note that variations in the anatomy and function of the glossopharyngeal nerve can occur. Some individuals may have a slightly different distribution of nerve fibers or variations in the size and shape of the nerve. These variations can influence the palpation results and should be taken into account when interpreting the findings.
Identifying Potential Abnormalities
While palpation of the glossopharyngeal nerve is generally used to assess its normal functioning, it can also reveal abnormalities or discrepancies that may suggest underlying issues. These abnormalities could include decreased sensation, changes in taste perception, or motor dysfunction of the muscles innervated by the glossopharyngeal nerve.
For example, if a patient reports a loss of taste sensation or difficulty swallowing, palpation of the glossopharyngeal nerve can help identify potential abnormalities. By applying gentle pressure and observing the patient’s response, healthcare professionals can gather valuable information about the nerve’s function and potential issues.
However, it is important to note that while palpation can provide valuable diagnostic information, it is not a stand-alone diagnostic tool. If any abnormalities are detected during the palpation process, it is crucial to consult with a healthcare professional for further evaluation and appropriate management. Additional tests and examinations may be necessary to confirm the presence of any underlying conditions or disorders.
In conclusion, interpreting the results of glossopharyngeal nerve palpation requires a thorough understanding of the normal anatomy, expected variations, and potential abnormalities. By considering the patient’s unique characteristics and utilizing additional diagnostic tools, healthcare professionals can accurately assess the functioning of the glossopharyngeal nerve and provide appropriate care.
Post-Palpation Procedures
Documenting Your Findings
Thorough documentation of the palpation procedure and its findings is vital for effective communication and future reference. Precise recording of the patient’s medical history, the techniques employed, and any abnormalities observed can aid in accurate diagnosis and treatment planning.
When documenting the details of the palpation procedure, it is important to include information such as the patient’s age, gender, and relevant medical conditions. This additional context can provide valuable insights into the patient’s overall health and help in identifying potential underlying causes of any abnormalities detected during palpation.
Furthermore, documenting the specific techniques employed during the palpation procedure is crucial for replicability and consistency. By clearly outlining the steps taken, future healthcare providers can refer to these records to ensure accurate and standardized assessments.
In addition to recording abnormalities observed, it is also important to note any normal findings. This comprehensive approach ensures that future comparisons can be made, helping to track the patient’s progress over time and identify any changes or patterns that may emerge.
Documenting the details of the palpation procedure in a clear and organized manner is essential for effective healthcare delivery and seamless continuity of care. By maintaining accurate and detailed records, healthcare professionals can collaborate more effectively, ensuring that the patient receives the best possible care.
Communicating Results to Patients
Once the palpation procedure is complete and the findings have been documented, it is essential to communicate these results to patients in a clear and understandable manner. This allows patients to become active participants in their own healthcare journey and fosters a strong doctor-patient relationship based on trust and shared decision-making.
When communicating the results to patients, it is important to use language that is easily understandable and free from medical jargon. This ensures that patients can fully comprehend the information being shared and make informed decisions about their health.
In addition to explaining the findings, it is crucial to provide patients with information on the potential implications of these findings. This empowers patients to understand the significance of the results and take appropriate actions, such as seeking further medical evaluation or following recommended treatment plans.
It is imperative to provide patients with accurate information while avoiding offering medical advice. Instead, healthcare professionals should focus on educating patients about their condition and available treatment options. Encouraging patients to consult with a qualified healthcare professional for further evaluation and guidance is essential to ensure their well-being and address any potential concerns or queries.
By effectively communicating the results of the palpation procedure to patients, healthcare professionals can establish a collaborative relationship, where patients feel empowered and actively involved in their own healthcare decisions. This patient-centered approach promotes better health outcomes and overall satisfaction with the healthcare experience.
Frequently Asked Questions about Glossopharyngeal Nerve Palpation
Glossopharyngeal nerve palpation is a medical procedure that involves the examination and assessment of the glossopharyngeal nerve, which is responsible for various functions in the head and neck region. This procedure is typically performed by trained healthcare professionals who have expertise in neurology or otolaryngology.
Risks and Complications of Palpation
Glossopharyngeal nerve palpation is generally a safe procedure when performed by a trained healthcare professional. However, as with any medical intervention, there may be minimal risks or complications.
During the palpation procedure, the patient may experience some discomfort. This discomfort is usually temporary and can be managed by the healthcare professional through proper technique and communication with the patient. Additionally, there is a possibility of a transient gag reflex, which may occur due to the stimulation of the glossopharyngeal nerve. However, this reflex is usually short-lived and does not cause any long-term complications.
In rare cases, there may be a risk of infection at the site of palpation. To minimize this risk, healthcare professionals follow strict aseptic precautions, ensuring that the procedure is performed in a sterile environment. By adhering to these precautions, the chances of infection can be significantly reduced.
When to Refer to a Specialist
If abnormalities or concerns arise during the glossopharyngeal nerve palpation procedure, it may be prudent to refer the patient to a specialist for further evaluation. Specialists, such as neurologists or otolaryngologists, possess the expertise to conduct more extensive diagnostic tests and provide appropriate management.
These specialists have in-depth knowledge of the glossopharyngeal nerve and its associated conditions. They can perform additional diagnostic procedures, such as imaging studies or nerve conduction tests, to further assess the nerve’s function and identify any underlying issues. By involving a specialist, healthcare professionals can ensure that the patient receives comprehensive care and appropriate treatment.
When in doubt, it is always best to err on the side of caution and involve a specialist to ensure optimal patient care and outcomes. The expertise of a specialist can provide valuable insights and guidance in managing complex cases related to the glossopharyngeal nerve.
By following the aforementioned steps and guidelines, healthcare professionals can effectively palpate the glossopharyngeal nerve, enabling them to gather valuable diagnostic information and contribute to a well-rounded approach to patient care. Always remember that palpation is just one component of a comprehensive assessment and should be supplemented with other diagnostic modalities to ensure accurate diagnosis and appropriate management.