The glossopharyngeal nerve is a crucial component of the cranial nerve system, responsible for innervating important structures in the oropharynx and providing sensory feedback from areas of the head and neck. Assessment of this nerve is vital for diagnosing potential pathologies and understanding patients’ overall health status. In this article, we will explore the various aspects involved in assessing the glossopharyngeal nerve, including its anatomy, functions, examination techniques, common pathologies, treatment options, and long-term care.
Understanding the Glossopharyngeal Nerve
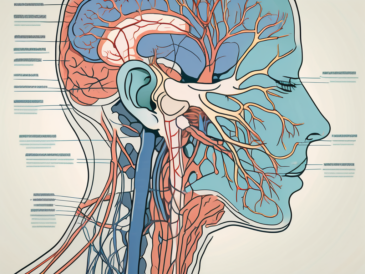
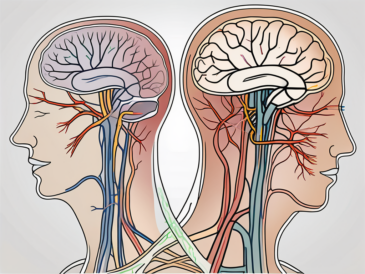
The glossopharyngeal nerve, also known as cranial nerve IX, is a fascinating component of the human nervous system. It arises from the medulla oblongata in the brainstem, a crucial region responsible for various vital functions. The nerve is comprised of both motor and sensory fibers, each playing a significant role in the overall functioning of the body.
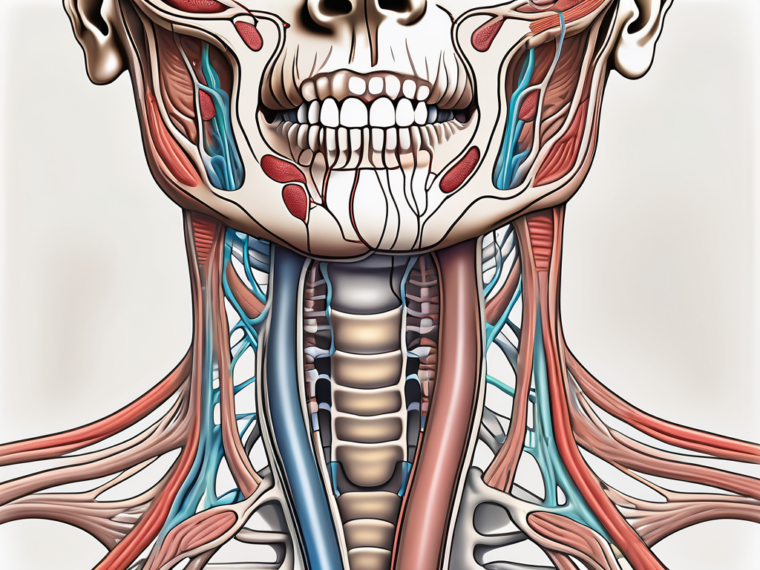
Anatomy of the Glossopharyngeal Nerve
Let’s delve deeper into the anatomy of the glossopharyngeal nerve. Emerging from the medulla oblongata, this nerve branches out into three main divisions, each with its own distinct purpose.
The first branch consists of motor fibers that innervate the stylopharyngeus muscle. This muscle is essential for swallowing and plays a crucial role in elevating the pharynx during speech. Without the proper functioning of this motor branch, these vital actions would become significantly impaired.
The second branch of the glossopharyngeal nerve is responsible for sensory functions. These sensory fibers provide taste sensation to the posterior third of the tongue, contributing to our ability to savor and enjoy the flavors of various foods. Additionally, they transmit general sensation from the oropharynx, tonsils, posterior pharyngeal wall, and even the middle ear cavity. This intricate network of sensory information allows us to perceive and respond to various stimuli in our environment.
Lastly, the glossopharyngeal nerve contains parasympathetic fibers that innervate the parotid gland. This gland, located near the ear, plays a crucial role in saliva production. The parasympathetic fibers of the glossopharyngeal nerve ensure that the parotid gland functions optimally, maintaining the necessary moisture in the mouth for proper digestion and oral health.
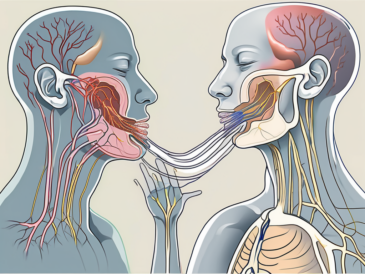
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve’s functions extend beyond its anatomical structure. This nerve is involved in a wide range of motor and sensory processes, all of which contribute to our overall well-being.
Motor fibers of the glossopharyngeal nerve allow us to perform essential actions such as swallowing and speaking. The stylopharyngeus muscle, innervated by these motor fibers, contracts to facilitate the movement of food and liquid through the pharynx and into the esophagus. Additionally, this muscle aids in elevating the pharynx during speech, allowing us to articulate words clearly and effectively.
The sensory fibers of the glossopharyngeal nerve are responsible for transmitting vital information from various regions of the head and neck. Taste sensation from the posterior third of the tongue is made possible through these sensory fibers, enabling us to experience the diverse flavors of the foods we consume. Furthermore, the general sensation transmitted by these fibers allows us to perceive touch, pressure, and pain in the oropharynx, tonsils, posterior pharyngeal wall, and middle ear cavity. This sensory feedback is crucial for our overall awareness and ability to respond to potential threats or discomfort.
Understanding the intricate functions and anatomy of the glossopharyngeal nerve provides us with a deeper appreciation for the complexity of the human body. The interplay between motor and sensory fibers within this nerve highlights the remarkable coordination required for our everyday actions and experiences.
Preparing for the Assessment
Before conducting the assessment, it is crucial to ensure that all necessary equipment is readily available. This includes a tongue depressor, penlight, cotton applicator, gloves, and a reflex hammer. These tools are essential for a comprehensive examination of the patient’s condition. Additionally, having access to an otoscope and laryngeal mirror can be beneficial when evaluating potential secondary complications or suspected abnormalities. These instruments allow for a closer examination of the patient’s ears, nose, throat, and larynx, providing valuable insights into their overall health.
Furthermore, it is important to note that the quality of the equipment used can greatly impact the accuracy of the assessment. Therefore, it is recommended to regularly check and maintain the condition of these tools, ensuring they are clean, functional, and in good working order. This not only ensures accurate results but also promotes the safety and well-being of the patient.
Necessary Equipment for the Examination
Prior to conducting the assessment, it is important to ensure that all necessary equipment is readily available. This includes a tongue depressor, penlight, cotton applicator, gloves, and a reflex hammer. These tools are essential for a comprehensive examination of the patient’s condition.
The tongue depressor is used to hold down the tongue, allowing for a clear view of the oral cavity and throat. It enables the healthcare professional to examine the tonsils, uvula, and other structures in the mouth, checking for any signs of inflammation, infection, or abnormalities.
The penlight is a small, portable flashlight that is used to illuminate the patient’s eyes, ears, nose, and throat. By shining the light into these areas, the healthcare professional can assess the pupillary response, check for redness or discharge in the eyes, and examine the nasal passages and throat for any signs of infection or inflammation.
The cotton applicator, also known as a swab, is used to collect samples for laboratory testing or to apply medication to specific areas. It is a versatile tool that allows for precise and controlled application, ensuring accurate results and effective treatment.
Gloves are an essential part of any medical examination to maintain proper hygiene and prevent the spread of infection. They protect both the healthcare professional and the patient from potential pathogens, ensuring a safe and sterile environment.
The reflex hammer, also known as a percussion hammer, is used to test the patient’s reflexes. By tapping specific areas of the body, such as the knee or elbow, the healthcare professional can assess the integrity of the nervous system and identify any abnormalities or potential underlying conditions.
Additionally, having access to an otoscope and laryngeal mirror can be beneficial when evaluating potential secondary complications or suspected abnormalities. These instruments allow for a closer examination of the patient’s ears, nose, throat, and larynx, providing valuable insights into their overall health.
Patient Preparation Guidelines
When preparing the patient for the assessment, it is essential to explain the procedure thoroughly, addressing any concerns they may have and obtaining informed consent. This open communication fosters trust and ensures that the patient feels comfortable and well-informed throughout the examination process.
Patients should be comfortably seated, with good lighting and a relaxed environment. A calm and soothing atmosphere promotes relaxation and cooperation, making the assessment more effective and accurate. It is important to ensure their head and neck are in a neutral position to allow for optimal examination. This position helps to align the patient’s airway and facilitates a clear view of the oral cavity and throat.
Furthermore, it is crucial to consider the patient’s comfort and privacy during the assessment. Providing a gown or draping to cover their body and maintaining their modesty is essential. Respecting their dignity and privacy not only promotes a positive patient experience but also encourages their cooperation and trust throughout the examination.
In conclusion, proper preparation for the assessment is crucial for obtaining accurate results and ensuring the well-being of the patient. By having the necessary equipment readily available and following patient preparation guidelines, healthcare professionals can conduct thorough examinations that provide valuable insights into the patient’s condition.
Conducting the Glossopharyngeal Nerve Assessment
When it comes to assessing the glossopharyngeal nerve, a systematic approach is essential. This ensures that all aspects of the nerve’s function are thoroughly evaluated. The assessment typically involves three main techniques: inspection, palpation, and specific tests to assess motor and sensory functions.
Inspection
During the inspection phase of the assessment, the healthcare professional carefully observes the patient’s oral cavity and throat. They look for any visible abnormalities or signs of dysfunction that may indicate issues with the glossopharyngeal nerve. This can include abnormalities in the movement of the uvula, the presence of asymmetry, or any signs of inflammation or infection.
Palpation
Palpation is another important technique used to assess the glossopharyngeal nerve. By gently applying pressure to specific areas of the throat and neck, the healthcare professional can evaluate the patient’s response and identify any areas of tenderness or abnormal sensations. This can provide valuable information about the nerve’s function and help pinpoint potential underlying issues.
Motor and Sensory Tests
In addition to inspection and palpation, specific tests are performed to assess the motor and sensory functions of the glossopharyngeal nerve. These tests may include assessing the patient’s ability to swallow, taste, and sense touch in certain areas of the throat and tongue. By evaluating these functions, healthcare professionals can gather more comprehensive information about the nerve’s overall health and identify any potential abnormalities.
It is important to note that while this article provides an overview of the assessment techniques, it is always recommended to consult with a healthcare professional for hands-on guidance. Conducting a thorough glossopharyngeal nerve assessment requires specialized knowledge and expertise to ensure accurate results.
Interpreting Physical Examination Findings
Once the assessment is complete, the healthcare professional must interpret the physical examination findings. This step is crucial in determining the presence of any abnormalities or potential pathologies related to the glossopharyngeal nerve.
Abnormalities observed during the assessment may suggest a range of conditions, including glossopharyngeal neuralgia, infections, tumors, or structural abnormalities. However, it is important to remember that physical examination findings alone are not sufficient for a definitive diagnosis. They must be analyzed in conjunction with the patient’s medical history, symptoms, and any additional diagnostic tests that may be required.
By considering all relevant factors, healthcare professionals can establish an accurate diagnosis and develop an appropriate treatment plan tailored to the patient’s specific needs.
In conclusion, conducting a glossopharyngeal nerve assessment requires a systematic approach that includes inspection, palpation, and specific tests to assess motor and sensory functions. Interpreting the physical examination findings is a critical step in identifying any abnormalities or potential pathologies related to the glossopharyngeal nerve. It is essential to consult with a healthcare professional for a comprehensive assessment and accurate diagnosis.
Common Pathologies of the Glossopharyngeal Nerve
The glossopharyngeal nerve is a crucial cranial nerve that plays a significant role in various functions related to the throat and taste sensations. When this nerve is damaged, it can lead to a range of symptoms that can greatly impact a patient’s quality of life.
Symptoms of Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can manifest with various symptoms, some of which may include throat pain, difficulty swallowing, altered taste sensations, earaches, hoarseness, or even syncope in severe cases. These symptoms can be distressing and require proper assessment and treatment to alleviate the patient’s discomfort.
Throat pain is a common symptom experienced by individuals with glossopharyngeal nerve damage. This pain can vary in intensity and may be localized or radiate to other areas of the head and neck. It can make swallowing difficult and uncomfortable, leading to a decreased appetite and potential weight loss.
Difficulty swallowing, known as dysphagia, is another significant symptom associated with glossopharyngeal nerve damage. This can make it challenging for individuals to consume both solid and liquid foods, leading to nutritional deficiencies and dehydration if not properly managed.
Altered taste sensations are also commonly reported by those with glossopharyngeal nerve damage. This can result in a distorted perception of taste, where certain foods may taste different or unpleasant. This can have a significant impact on an individual’s enjoyment of meals and overall dietary habits.
Earaches can occur as a result of glossopharyngeal nerve damage. The nerve fibers of the glossopharyngeal nerve are closely related to the ear, and any disruption in its function can lead to referred pain in the ear. This can cause discomfort and may require additional evaluation by an ear, nose, and throat specialist.
Hoarseness is another symptom that may arise from glossopharyngeal nerve damage. The nerve plays a role in controlling the muscles responsible for vocalization, and any impairment can result in changes in voice quality, pitch, and volume. This can affect an individual’s ability to communicate effectively and may require speech therapy interventions.
In severe cases, glossopharyngeal nerve damage can even lead to syncope, which is a temporary loss of consciousness. This occurs due to the nerve’s involvement in regulating blood pressure and heart rate. Syncope episodes can be alarming and require immediate medical attention to identify and address the underlying cause.
Conditions Affecting the Glossopharyngeal Nerve
Multiple conditions can affect the glossopharyngeal nerve, each with its own set of implications and treatment considerations. Understanding these conditions is vital for accurate assessment, differential diagnosis, and appropriate treatment planning.
Glossopharyngeal neuralgia is a condition characterized by recurring episodes of severe pain in the throat, ear, and base of the tongue. It occurs due to irritation or compression of the glossopharyngeal nerve, leading to intense and debilitating pain. Treatment options for glossopharyngeal neuralgia may include medications, nerve blocks, or surgical interventions.
Infections such as tonsillitis or pharyngitis can also affect the glossopharyngeal nerve. These inflammatory conditions can lead to swelling and irritation of the throat, potentially causing damage to the nerve fibers. Prompt diagnosis and appropriate antibiotic therapy are essential in managing these infections and preventing further complications.
Tumors can also impact the glossopharyngeal nerve, either by directly compressing it or infiltrating the surrounding tissues. Tumors can be benign or malignant and may require surgical removal, radiation therapy, or chemotherapy, depending on their nature and extent.
Trauma, such as head or neck injuries, can result in glossopharyngeal nerve damage. The nerve can be stretched, compressed, or severed, leading to a range of symptoms depending on the severity of the injury. Rehabilitation and supportive care are crucial in promoting nerve healing and restoring optimal function.
In conclusion, the glossopharyngeal nerve is susceptible to various pathologies that can significantly impact an individual’s well-being. Recognizing the symptoms associated with glossopharyngeal nerve damage and understanding the conditions that can affect this nerve are crucial in providing appropriate assessment, diagnosis, and treatment for affected individuals.
Treatment Options for Glossopharyngeal Nerve Disorders
Non-Surgical Treatment Methods
Non-surgical treatment methods are often the first line of approach for glossopharyngeal nerve disorders. This may include medications to control pain, physical therapy to improve swallowing and speech function, and lifestyle modifications to minimize triggering factors. It is imperative for patients to consult with a healthcare professional to determine the most suitable treatment plan based on their individual needs.
Surgical Treatment Methods
In some cases, when non-surgical interventions prove ineffective or if there is an underlying structural issue, surgical treatment may be considered. Surgical options range from nerve blocks and neurolysis to microvascular decompression or even neurectomy. Each method carries its own potential risks and benefits, and a thorough evaluation of patient-specific factors should guide the decision-making process.
Follow-up and Long-Term Care
Monitoring Patient Progress
After assessment and treatment, it is crucial to monitor patients’ progress regularly. This may involve follow-up visits to evaluate treatment efficacy, assess any potential complications or side effects, and implement additional strategies as necessary. Patient compliance and engagement in the rehabilitation process play a pivotal role in achieving optimal outcomes.
Rehabilitation and Therapy Options
Depending on the specific glossopharyngeal nerve disorder and associated impairments, rehabilitation and therapy options may be beneficial to aid in recovery and improve overall quality of life. These can include speech therapy, swallowing exercises, and strategies to manage pain and discomfort. Consulting with a specialized healthcare professional, such as a speech-language pathologist or physiotherapist, can provide valuable guidance in developing an individualized therapy plan.
In conclusion, assessing the glossopharyngeal nerve involves a comprehensive evaluation of its anatomy, functions, physical examination techniques, common pathologies, treatment options, and long-term care. While this article provides a general overview of the topic, it is essential to seek professional advice and expertise to ensure accurate assessment and appropriate treatment. By understanding the intricacies of assessing the glossopharyngeal nerve, healthcare professionals can provide superior care and improve patients’ quality of life.