The glossopharyngeal nerve is a crucial component of the human nervous system, responsible for numerous functions that are vital to our overall well-being. In this article, we will delve into the intricacies of assessing the glossopharyngeal nerve, exploring its anatomy, functions, and the step-by-step process involved in evaluating its health.
Understanding the Glossopharyngeal Nerve
Anatomy of the Glossopharyngeal Nerve
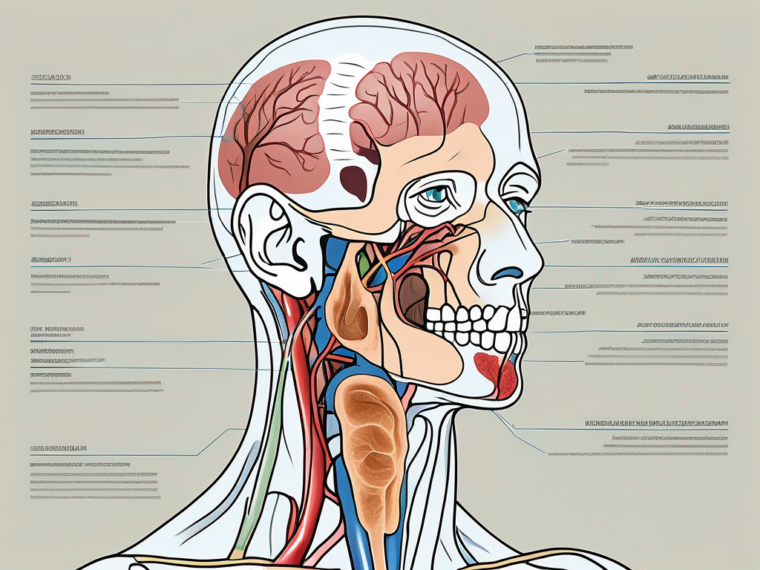
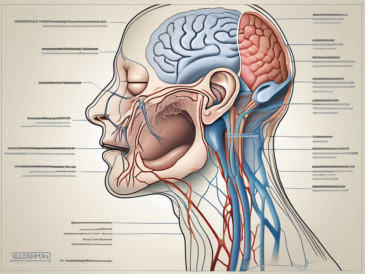
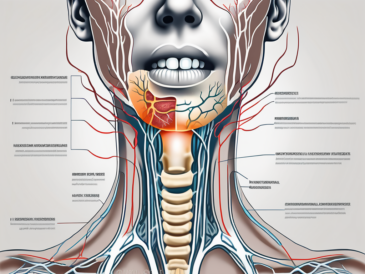
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve cranial nerves originating from the brainstem. Emerging from the jugular foramen, it consists of both motor and sensory fibers.
The motor fibers of the glossopharyngeal nerve are involved in controlling the muscles responsible for swallowing and speech. These muscles work in harmony to facilitate the complex process of swallowing, allowing us to consume and digest food efficiently. Additionally, they play a crucial role in speech production, enabling us to communicate and express ourselves through language.
On the other hand, the sensory fibers of the glossopharyngeal nerve innervate the posterior third of the tongue, the oropharynx, and the tonsils. These sensory signals are essential for our ability to taste and perceive flavors. They allow us to enjoy the diverse range of tastes that make eating a pleasurable experience.
Functions of the Glossopharyngeal Nerve
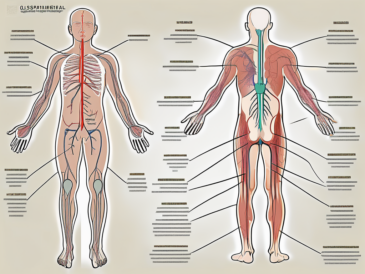
The glossopharyngeal nerve serves a multitude of essential functions, ranging from the perception of taste to the regulation of blood pressure. It facilitates the transmission of sensory information from the areas it innervates and plays a pivotal role in maintaining the body’s homeostasis.
One of the key functions of the glossopharyngeal nerve is its involvement in the regulation of blood pressure. It contains specialized receptors called baroreceptors, which detect changes in blood pressure. When these receptors sense a decrease in blood pressure, they send signals to the brain, triggering a response to increase blood pressure and maintain adequate circulation throughout the body.
In addition to its role in blood pressure regulation, the glossopharyngeal nerve is responsible for transmitting taste signals from the posterior third of the tongue. These taste signals are essential for our ability to savor and appreciate the flavors that enrich our lives. From the sweetness of a ripe strawberry to the savory umami taste of a perfectly cooked steak, the glossopharyngeal nerve allows us to experience the full spectrum of tastes and enjoy the culinary delights of the world.
Furthermore, the glossopharyngeal nerve plays a vital role in the reflexes involved in swallowing. When food or liquid enters the back of the throat, sensory receptors in the oropharynx are stimulated, sending signals through the glossopharyngeal nerve to the brain. In response, the brain coordinates the contraction of the muscles involved in swallowing, ensuring that the food or liquid is safely transported from the mouth to the stomach.
Overall, the glossopharyngeal nerve is a remarkable cranial nerve that contributes to various essential functions in the human body. From enabling us to taste and enjoy flavors to regulating blood pressure and facilitating the process of swallowing, this nerve plays a crucial role in our daily lives.
Preparing for the Assessment
Before embarking on the assessment of the glossopharyngeal nerve, it is imperative to ensure that you have the necessary tools at your disposal and that the patient is adequately prepared for the examination.
Necessary Tools for Assessment
To assess the glossopharyngeal nerve, the following tools are essential:
- A good light source for optimal visualization
- A tongue depressor to facilitate examination of the oropharynx
- An otoscope to assess the condition of the tonsils, if required
- A neurological reflex hammer for testing reflexes, if necessary
When it comes to assessing the glossopharyngeal nerve, having the right tools can make a significant difference in the accuracy and effectiveness of the examination. A good light source is crucial for optimal visualization of the oropharynx, allowing you to identify any abnormalities or irregularities that may be indicative of glossopharyngeal nerve dysfunction.
The tongue depressor is another indispensable tool for this assessment. It enables you to gently depress the tongue, providing a clear view of the oropharynx and allowing for a thorough examination of the glossopharyngeal nerve. With the aid of a tongue depressor, you can assess the movement and sensation of the posterior third of the tongue, the soft palate, and the pharynx.
In some cases, it may be necessary to use an otoscope during the assessment of the glossopharyngeal nerve. This tool allows for a closer examination of the tonsils, which can provide valuable insights into the overall health and function of the glossopharyngeal nerve. By carefully inspecting the tonsils, you can detect any signs of inflammation, infection, or other abnormalities that may be affecting the nerve’s function.
Lastly, a neurological reflex hammer may be required during the assessment to test the gag reflex, which is mediated by the glossopharyngeal nerve. By gently tapping the back of the throat, you can elicit the gag reflex and evaluate its strength and symmetry, providing further information about the functioning of the glossopharyngeal nerve.
Patient Preparation Guidelines
Prior to the assessment, it is crucial to prepare the patient adequately. Clearly explain the purpose and procedure of the examination, addressing any concerns or fears they may have.
Effective communication with the patient is key to ensuring their comfort and cooperation during the assessment. Take the time to establish rapport and build trust, allowing the patient to feel at ease and more willing to participate in the examination process. Encourage them to ask questions and express any concerns they may have, providing reassurance and clarification as needed.
Furthermore, it is important to gather relevant medical history from the patient before proceeding with the assessment. Inquire about any known allergies or previous adverse experiences during similar assessments. This information can help you tailor the examination to the patient’s specific needs, ensuring their safety and well-being throughout the process.
In addition to medical history, it is essential to inquire about the patient’s recent food and beverage intake. Certain substances can affect taste perception, potentially influencing the results of the assessment. To obtain accurate and reliable findings, advise the patient to refrain from consuming food or beverages that may alter taste perception immediately before the examination.
By following these patient preparation guidelines, you can create a conducive environment for the assessment of the glossopharyngeal nerve. Taking the time to establish rapport, gather relevant medical history, and ensure the patient’s comfort and cooperation will contribute to a successful and informative examination.
Step-by-Step Assessment Process
Now that we have familiarized ourselves with the necessary groundwork, we can explore the step-by-step process involved in assessing the glossopharyngeal nerve.
The glossopharyngeal nerve is a crucial cranial nerve responsible for various functions, including taste perception, swallowing, and speech. Assessing its function is essential in diagnosing potential issues and providing appropriate treatment.
Initial Observations
The assessment begins with a visual inspection of the patient’s external features, aiming to identify any abnormalities or asymmetries that may indicate underlying issues. Observe the patient’s facial movements, speech patterns, and overall behavior.
Take note of any signs of difficulty swallowing, changes in voice quality, or alterations in taste perception that could be indicative of glossopharyngeal nerve dysfunction.
For example, if the patient demonstrates difficulty in swallowing, it may suggest impaired motor function of the glossopharyngeal nerve, affecting the coordination of the muscles involved in the swallowing process.
Similarly, alterations in taste perception, such as the inability to detect certain tastes or experiencing a persistent metallic taste, may indicate sensory dysfunction of the glossopharyngeal nerve.
Physical Examination Techniques
The physical examination phase involves a comprehensive evaluation of the structures innervated by the glossopharyngeal nerve. This typically encompasses:
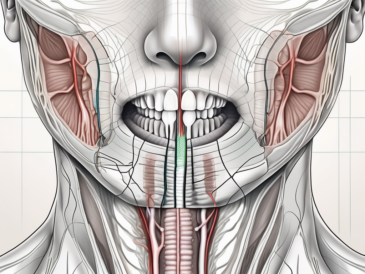
- Inspection of the oral cavity, including examination of the tonsils and oropharynx for abnormalities or inflammation
- Testing the gag reflex, which is mediated by the glossopharyngeal nerve, by gently stimulating the back of the throat with a tongue depressor or cotton swab
- Evaluating taste perception using taste stimuli such as sweet, salty, sour, and bitter substances
- Assessing the patient’s ability to swallow and speak clearly to determine the function of the motor fibers
During the inspection of the oral cavity, it is important to pay attention to any redness, swelling, or ulcerations that may indicate inflammation or infection. Abnormalities in the tonsils, such as enlargement or the presence of pus, may also provide valuable diagnostic clues.
Testing the gag reflex involves stimulating the glossopharyngeal nerve by gently touching the back of the throat. A normal response would involve the contraction of the muscles in the throat, while an absent or weakened response may indicate glossopharyngeal nerve dysfunction.
Evaluating taste perception is another crucial aspect of assessing the glossopharyngeal nerve. By using taste stimuli, such as sweet, salty, sour, and bitter substances, the healthcare provider can determine if the patient’s taste buds are functioning properly. Any discrepancies in taste perception may suggest sensory impairment of the glossopharyngeal nerve.
Assessing the patient’s ability to swallow and speak clearly provides insights into the motor function of the glossopharyngeal nerve. Difficulties in swallowing or slurred speech may indicate underlying issues affecting the nerve’s motor fibers.
These examination techniques, when performed meticulously, provide valuable insights into the integrity of the glossopharyngeal nerve and its associated functions. By identifying any abnormalities or dysfunctions, healthcare professionals can develop appropriate treatment plans to address the patient’s specific needs.
Interpreting the Assessment Results
Upon completion of the assessment, it is crucial to interpret the findings carefully and accurately. This step involves distinguishing between normal and abnormal results and recognizing potential disorders or conditions that may affect the glossopharyngeal nerve.
When interpreting the assessment results, it is important to consider various factors that may influence the findings. These factors can include the patient’s age, medical history, and any previous injuries or surgeries they may have had. Additionally, it is essential to take into account the specific assessment techniques used and any limitations they may have.
Normal vs. Abnormal Findings
A thorough understanding of what constitutes normal findings is imperative to effectively identify abnormal results during the assessment. Normal findings for the glossopharyngeal nerve assessment may include intact gag reflex, normal swallowing function, and absence of any pain or discomfort in the throat area.
However, it is important to note that abnormal findings do not always indicate a serious underlying condition. Sometimes, certain factors such as anxiety or temporary inflammation can cause temporary abnormalities in the assessment results. Therefore, it is essential to consider the overall clinical picture and consult with a medical professional to determine the significance of the findings.
Consulting with a medical professional experienced in neurology is highly recommended to ensure an accurate diagnosis and appropriate treatment plan. They can provide valuable insights and help differentiate between benign abnormalities and potential disorders affecting the glossopharyngeal nerve.
Potential Disorders and Conditions
The glossopharyngeal nerve can be affected by various disorders and conditions, including glossopharyngeal neuralgia, tumors, infections, and trauma. Glossopharyngeal neuralgia is a rare condition characterized by severe, recurring pain in the throat, ear, and tongue. Tumors affecting the glossopharyngeal nerve can be benign or malignant and may require surgical intervention or other treatments.
Infections, such as tonsillitis or pharyngitis, can also lead to inflammation and temporary dysfunction of the glossopharyngeal nerve. Trauma, such as a direct injury to the throat or neck area, can cause damage to the nerve and result in various symptoms.
Each condition presents unique symptoms and requires individualized management. Treatment options may include medications to manage pain and inflammation, physical therapy to improve swallowing function, or surgical interventions to address underlying causes such as tumors or nerve compression.
If an abnormality is suspected or if the patient presents with symptoms indicative of glossopharyngeal nerve dysfunction, it is vital to consult with a healthcare provider to conduct further diagnostic tests and develop an appropriate treatment approach. The healthcare provider may recommend imaging studies, such as an MRI or CT scan, to evaluate the structures surrounding the glossopharyngeal nerve and identify any potential abnormalities.
In conclusion, interpreting the assessment results for the glossopharyngeal nerve requires careful consideration of normal and abnormal findings, consultation with a medical professional, and awareness of potential disorders and conditions that may affect the nerve. By taking a comprehensive approach, healthcare providers can ensure accurate diagnoses and provide appropriate treatment plans for patients experiencing glossopharyngeal nerve dysfunction.
Safety Measures During Assessment
While carrying out the assessment, it is crucial to prioritize patient safety and comfort. Implementing safety measures and considering potential risks is paramount to a successful examination.
Precautions to Avoid Injury
Adhere to strict aseptic techniques to minimize the risk of infection during the assessment process. Additionally, exercise caution while using any instruments to prevent injury to the patient.
Ensure that all tools are clean and sterilized before use, and dispose of them appropriately following the examination.
Ensuring Patient Comfort
Throughout the assessment, prioritize the patient’s comfort and well-being. Establish open communication, reassuring the patient and encouraging them to ask questions or voice any concerns they may have.
Explain each step of the examination before performing it, ensuring the patient’s informed consent. By creating a supportive and caring environment, you can mitigate anxiety and enhance the overall patient experience.
Post-Assessment Procedures
Following the assessment of the glossopharyngeal nerve, it is essential to conclude the process with specific post-assessment procedures.
Communicating Results to the Patient
Take the time to communicate the assessment results to the patient in a clear and understandable manner. Address any concerns or questions they may have, ensuring they are well-informed about the findings.
However, it is important to emphasize that as an article writer, I cannot provide personalized medical advice. Therefore, it is crucial to advise the patient to consult with a qualified healthcare professional to discuss the assessment results and any subsequent steps that may need to be taken.
Next Steps and Follow-Up
After communicating the assessment results, collaborate with the patient’s healthcare provider to determine the best course of action. Depending on the findings, further diagnostic tests or specialized consultations may be required.
Encourage the patient to adhere to any recommended follow-up appointments and emphasize the importance of regular check-ups to monitor their condition effectively.
Frequently Asked Questions about Glossopharyngeal Nerve Assessment
Common Misconceptions
There are several common misconceptions surrounding glossopharyngeal nerve assessment. One prevalent misconception is that this assessment can be performed solely by individuals without appropriate medical training. However, due to the complexity of the examination and the potential for misinterpretation, it is crucial to involve healthcare professionals experienced in neurology.
Another misconception is that abnormalities detected during the assessment necessarily indicate a severe or untreatable condition. While abnormalities may be indicative of an underlying issue, only a qualified healthcare professional can provide an accurate diagnosis and determine the appropriate course of action.
Expert Tips for Accurate Assessment
Based on experience and expertise, experts recommend the following tips for ensuring an accurate glossopharyngeal nerve assessment:
- Thoroughly familiarize yourself with the anatomy and function of the glossopharyngeal nerve before performing the assessment.
- Establish a comfortable and supportive environment to maximize the patient’s cooperation and minimize anxiety.
- Maintain meticulous attention to detail during the examination process, noting any abnormalities or variances from what is expected.
- Regularly update your knowledge and skills through continuing education to stay current with the latest advancements in neurological assessment techniques.
By adhering to these expert tips, healthcare professionals can enhance the accuracy and effectiveness of their glossopharyngeal nerve assessments, ultimately benefiting patient care.
In conclusion, assessing the glossopharyngeal nerve is a vital aspect of neurological evaluation. By understanding the anatomy, functions, and step-by-step assessment process, healthcare professionals can identify potential abnormalities and facilitate appropriate management strategies. It is important to recognize the limitations of this article and the need for consultation with a qualified medical professional when interpreting assessment findings and determining further steps.