The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a crucial role in various functions of the head and neck. Testing for glossopharyngeal nerve damage involves a comprehensive assessment of its anatomy, functions, and symptoms. Additionally, diagnostic procedures help evaluate its integrity and identify any potential issues. In this article, we will explore the various aspects of testing for glossopharyngeal nerve damage, including understanding its anatomy, recognizing symptoms, diagnostic procedures, interpreting test results, treatment options, and prevention strategies.
Understanding the Glossopharyngeal Nerve
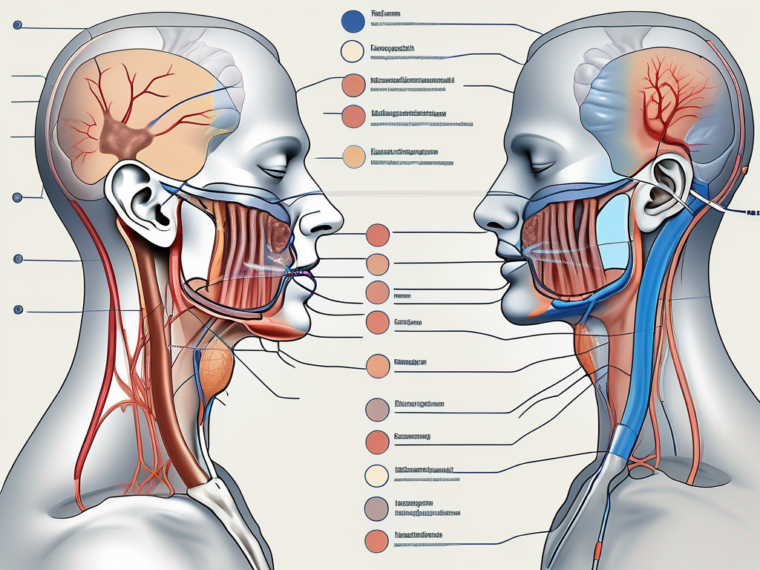
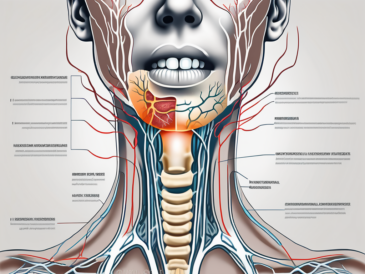
The glossopharyngeal nerve is a crucial component of the human nervous system. It consists of both sensory and motor fibers, originating from the medulla oblongata, a vital part of the brainstem responsible for various essential functions. These fibers then travel through the jugular foramen, a small opening in the base of the skull, to reach their respective destinations.
One of the primary roles of the glossopharyngeal nerve is to provide sensory feedback from specific regions in the oral and pharyngeal cavity. This includes the back third of the tongue, which plays a significant role in taste perception. Without the glossopharyngeal nerve, our ability to savor the flavors of our favorite foods would be greatly diminished.
In addition to taste perception, the glossopharyngeal nerve also contributes to the function of swallowing. It innervates the muscles involved in the swallowing process, ensuring the smooth movement of food and liquids from the mouth to the esophagus. Without this nerve, the act of swallowing would become a challenging and potentially dangerous task.
Furthermore, the glossopharyngeal nerve plays a role in the secretion of saliva. Saliva is essential for the lubrication of the oral cavity, aiding in the breakdown and digestion of food. The glossopharyngeal nerve stimulates the salivary glands, ensuring the proper production and release of saliva.
Anatomy of the Glossopharyngeal Nerve
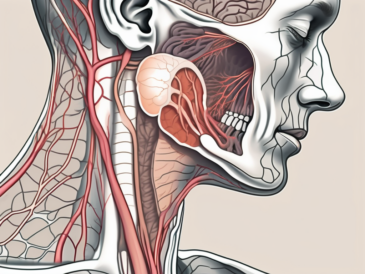
To understand the glossopharyngeal nerve better, it is essential to delve into its intricate anatomy. Emerging from the medulla oblongata, the nerve initially appears as a collection of nerve fibers. These fibers then exit the skull through the jugular foramen, alongside other cranial nerves, in a complex network of neural pathways.
Once outside the skull, the glossopharyngeal nerve branches out to innervate specific regions within the oral and pharyngeal cavity. It sends sensory fibers to the back third of the tongue, allowing us to perceive taste sensations. Additionally, it provides sensation to the soft palate, the tonsils, and the pharynx, contributing to the complex reflexes involved in swallowing and the gag reflex.
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve serves multiple important functions, making it an indispensable part of our daily lives. Its sensory fibers carry crucial information from the back third of the tongue, ensuring our ability to enjoy the diverse flavors of the foods we consume. Without this nerve, our taste buds would be rendered ineffective, and the culinary experience would be significantly diminished.
In addition to taste perception, the glossopharyngeal nerve plays a vital role in the regulation of blood pressure. It contains specialized receptors called baroreceptors, located in the carotid sinus, which detect changes in blood pressure. These receptors send signals via the glossopharyngeal nerve to the brain, allowing for the necessary adjustments to maintain optimal blood pressure levels.
Furthermore, the glossopharyngeal nerve is involved in the complex reflexes associated with swallowing and the gag reflex. It ensures the coordination of various muscles in the oral and pharyngeal cavity, facilitating the safe passage of food and liquids down the esophagus. Without the glossopharyngeal nerve, the act of swallowing would become a perilous endeavor, potentially leading to choking or aspiration.
Overall, the glossopharyngeal nerve is a remarkable component of our nervous system. Its sensory and motor functions contribute to our ability to taste, swallow, and maintain proper blood pressure levels. Without this nerve, our everyday experiences, from enjoying a delicious meal to maintaining our health, would be significantly compromised.
Symptoms of Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can manifest in various physical and sensory symptoms. It is important to recognize these signs in order to identify the need for further testing and evaluation.
Physical Symptoms
Physical symptoms of glossopharyngeal nerve damage may include difficulty swallowing (dysphagia), hoarseness of voice, weakness or paralysis of the muscles involved in speech and swallowing, and impaired gag reflex. In severe cases, there may be atrophy or wasting of certain muscles in the head and neck region.
Difficulty swallowing, known as dysphagia, is a common physical symptom of glossopharyngeal nerve damage. This can make it challenging to eat and drink, leading to weight loss and malnutrition if not properly managed. Hoarseness of voice may also occur, as the muscles responsible for vocalization may be affected.
Weakness or paralysis of the muscles involved in speech and swallowing can significantly impact an individual’s ability to communicate and consume food and liquids. This can result in the need for alternative methods of communication and specialized diets or feeding tubes to ensure proper nutrition.
The impaired gag reflex is another physical symptom that may arise from glossopharyngeal nerve damage. The gag reflex helps protect the airway by triggering a reflexive response to prevent choking. When this reflex is compromised, there is an increased risk of aspiration and respiratory complications.
In severe cases of glossopharyngeal nerve damage, atrophy or wasting of certain muscles in the head and neck region may occur. This can lead to visible changes in the appearance of the affected area, such as sunken cheeks or a noticeable reduction in muscle mass.
Sensory Symptoms
Sensory symptoms associated with glossopharyngeal nerve damage include decreased or altered taste sensation in the back of the tongue, a feeling of something stuck in the throat, and reduced sensation in the pharynx and tonsils. Some individuals may also experience pain in the throat and tongue.
When the glossopharyngeal nerve is damaged, the taste sensation in the back of the tongue may be affected. This can result in a decreased ability to taste certain flavors or an altered perception of taste. Individuals may find that foods they once enjoyed now taste different or have a diminished taste experience.
A feeling of something stuck in the throat, also known as globus sensation, can be a distressing sensory symptom of glossopharyngeal nerve damage. This sensation can cause discomfort and anxiety, as individuals may constantly feel the need to clear their throat or swallow in an attempt to alleviate the feeling.
Reduced sensation in the pharynx and tonsils is another sensory symptom that may occur. This can lead to difficulties in detecting and responding to potential irritants or foreign objects in the throat, increasing the risk of aspiration and choking.
In addition to altered taste and globus sensation, some individuals with glossopharyngeal nerve damage may experience pain in the throat and tongue. This pain can range from mild discomfort to severe, sharp sensations, making it difficult to eat, speak, or perform daily activities comfortably.
Diagnostic Procedures for Glossopharyngeal Nerve Testing
When glossopharyngeal nerve damage is suspected, several diagnostic procedures can help evaluate its integrity and identify potential issues. These procedures are essential for diagnosing the condition and determining the most appropriate treatment plan.
Medical History and Physical Examination
During the medical history assessment, the healthcare provider will inquire about the individual’s symptoms, their duration, and any potential triggers or underlying medical conditions. A thorough physical examination will also be performed to assess for any visible abnormalities or signs of nerve damage.
The medical history assessment is a crucial step in the diagnostic process as it helps the healthcare provider understand the patient’s symptoms and their impact on daily life. By gathering information about the duration and triggers of the symptoms, the healthcare provider can gain insights into the possible causes of glossopharyngeal nerve damage. Additionally, the medical history assessment may reveal any underlying medical conditions that could contribute to nerve dysfunction.
During the physical examination, the healthcare provider will carefully examine the patient’s head, neck, and throat. They will look for any visible abnormalities, such as muscle weakness or atrophy, that may indicate glossopharyngeal nerve damage. The provider may also perform specific tests, such as assessing the patient’s ability to swallow or evaluating their gag reflex, to further evaluate the function of the glossopharyngeal nerve.
Imaging Techniques
Imaging techniques, such as magnetic resonance imaging (MRI), may be employed to visualize the brainstem, the involved cranial nerves, and any potential structural abnormalities. MRI scans provide detailed images that help identify the location and extent of nerve damage.
An MRI scan is a non-invasive procedure that uses powerful magnets and radio waves to create detailed images of the body’s internal structures. In the case of glossopharyngeal nerve testing, an MRI can help identify any structural abnormalities, such as tumors or lesions, that may be compressing or damaging the nerve. The images obtained from an MRI can provide valuable information to guide treatment decisions and determine the most appropriate course of action.
During an MRI, the patient lies on a table that slides into a large, tunnel-like machine. It is important for the patient to remain still during the procedure to ensure clear and accurate images. Some patients may feel claustrophobic inside the MRI machine, but measures can be taken to help them feel more comfortable, such as providing earplugs or playing calming music.
Electrophysiological Testing
Electrophysiological testing involves the measurement of electrical signals generated by nerve activity. This testing can help evaluate the conduction of nerve impulses along the glossopharyngeal nerve and determine if any blockages or abnormalities exist. Electromyography (EMG) and nerve conduction studies (NCS) are commonly used electrophysiological techniques.
Electromyography (EMG) is a diagnostic procedure that involves the insertion of small, needle-like electrodes into the muscles. These electrodes detect and record the electrical activity produced by the muscles at rest and during contraction. In the case of glossopharyngeal nerve testing, EMG can help assess the function of the muscles involved in swallowing and speech, which are controlled by the glossopharyngeal nerve.
Nerve conduction studies (NCS) measure the speed and strength of electrical signals as they travel along the nerves. During this procedure, small electrodes are placed on the skin over the nerve being tested. A mild electrical impulse is then applied to the nerve, and the resulting electrical activity is recorded. NCS can help determine if there are any disruptions or abnormalities in the conduction of nerve impulses along the glossopharyngeal nerve.
Both EMG and NCS are safe and well-tolerated procedures that provide valuable information about the function of the glossopharyngeal nerve. The results of these tests can help confirm a diagnosis of glossopharyngeal nerve damage and guide treatment decisions.
Interpreting Test Results
Interpreting the results of glossopharyngeal nerve testing requires expertise and familiarity with the normal functioning of the nerve. Understanding the significance of the findings is crucial in order to make accurate diagnoses and determine appropriate treatment strategies.
The glossopharyngeal nerve, also known as the ninth cranial nerve, plays a vital role in various functions of the head and neck. It is responsible for transmitting sensory information from the back of the throat, tongue, and middle ear to the brain. Additionally, it controls the muscles involved in swallowing and helps regulate blood pressure.
When evaluating the results of glossopharyngeal nerve testing, it is important to consider both normal and abnormal findings. In individuals with a healthy glossopharyngeal nerve, the results of testing should show normal nerve conduction and appropriate responses to various stimuli.
Normal findings may include a consistent and timely transmission of nerve impulses, indicating that the nerve is functioning properly. Responses to sensory stimuli, such as taste or touch, should be present and within the expected range.
On the other hand, abnormal findings may indicate underlying issues with the glossopharyngeal nerve. These abnormalities can manifest as a decrease in nerve conduction velocity, meaning that the nerve impulses are traveling slower than usual. Reduced or absent responses to sensory stimuli may also be observed, suggesting a disruption in the transmission of signals along the nerve pathway.
In some cases, electrophysiological testing may reveal abnormal electrical activity in the affected glossopharyngeal nerve. This can be indicative of nerve damage or dysfunction, which may require further investigation and treatment.
Potential Complications and Risks
It is essential to be aware that diagnostic procedures, such as electrophysiological testing, may carry some risks and possible complications. While these risks are generally rare, it is important to discuss them with a healthcare professional prior to undergoing any testing.
During the procedure, some individuals may experience discomfort or pain as the electrodes are placed on the skin or inserted into the muscles. This discomfort is usually temporary and subsides once the testing is complete.
In rare cases, temporary muscle weakness or numbness may occur as a result of the electrical stimulation used during the testing. This is typically transient and resolves on its own without any long-term effects.
Additionally, there is a minimal risk of infection associated with any invasive procedure. However, healthcare professionals take strict precautions to minimize this risk by ensuring proper sterilization techniques and using sterile equipment.
It is important to communicate any concerns or questions regarding the potential risks and complications of glossopharyngeal nerve testing with your healthcare provider. They can provide you with the necessary information and address any specific concerns you may have.
Treatment Options for Glossopharyngeal Nerve Damage
Once glossopharyngeal nerve damage is diagnosed, treatment options focus on managing the symptoms and addressing any underlying cause. The most appropriate treatment plan will depend on the severity of the damage and the specific symptoms experienced by the individual.
Medications and Therapies
In some cases, medications may be prescribed to alleviate symptoms associated with glossopharyngeal nerve damage. These may include pain medications, muscle relaxants, and medications to enhance swallowing or regulate blood pressure. Additionally, physical or speech therapy may be recommended to improve swallowing and speech function.
Surgical Interventions
In severe cases of glossopharyngeal nerve damage, surgical interventions may be considered. These procedures aim to repair or restore the damaged nerve or address any underlying conditions causing the damage. Surgical options include nerve grafts, nerve decompression surgeries, or procedures to remove any compressive structures.
Prevention and Management of Glossopharyngeal Nerve Damage
While it may not always be possible to prevent glossopharyngeal nerve damage, there are certain measures individuals can take to minimize the risk and manage the condition effectively if it occurs.
Lifestyle Modifications
Lifestyle modifications can play a key role in preventing or managing glossopharyngeal nerve damage. These may include adopting a healthy diet rich in nutrients, avoiding excessive alcohol consumption, maintaining proper hydration, and practicing good oral hygiene. It is also important to avoid activities that may put undue stress or strain on the head and neck region, such as excessive shouting or straining during bowel movements.
Regular Check-ups and Monitoring
Regular check-ups with a healthcare provider are essential for individuals at risk of glossopharyngeal nerve damage or those already diagnosed with the condition. Routine monitoring can help detect any changes in symptoms or the need for adjustments to the treatment plan. Consultation with a healthcare provider and adherence to their recommendations are crucial for effectively managing glossopharyngeal nerve damage.
Overall, testing for glossopharyngeal nerve damage involves a multi-faceted approach, including understanding its anatomy and functions, recognizing symptoms, performing diagnostic procedures, interpreting test results, determining treatment options, and implementing preventive strategies. Receiving timely and accurate testing, as well as appropriate medical care, is vital in managing glossopharyngeal nerve damage and improving the individual’s quality of life. Consultation with a healthcare professional is strongly encouraged for anyone with concerns regarding their glossopharyngeal nerve function or the presence of any related symptoms.