The glossopharyngeal nerve is a crucial cranial nerve that plays a vital role in various sensory and motor functions of the head and neck. Testing the function of this nerve can provide valuable diagnostic information and help determine the underlying cause of certain symptoms. In this article, we will delve into the details of how to test the glossopharyngeal nerve, including understanding its anatomy, preparing for the test, performing the procedure, interpreting the results, potential complications and risks, as well as post-test care and follow-up. It is important to note that this article is informational in nature and does not constitute medical advice. If you suspect any issues with your glossopharyngeal nerve function or have concerns, it is recommended to consult with a qualified medical professional.
Understanding the Glossopharyngeal Nerve
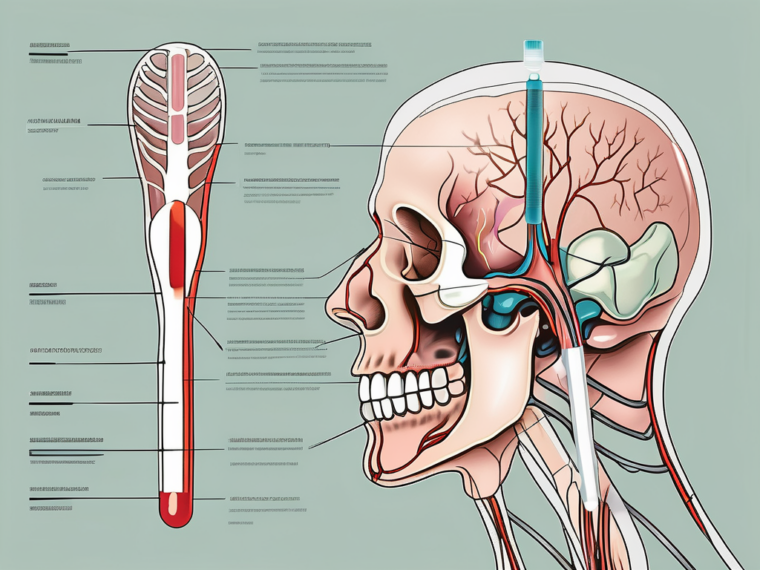
The glossopharyngeal nerve, also known as cranial nerve IX, is the ninth cranial nerve emerging from the brainstem. It consists of both motor and sensory fibers. The motor fibers innervate muscles involved in swallowing, while the sensory fibers carry information related to taste, sensation, and reflexes from the throat, tongue, and other areas of the oral cavity.
The anatomy of the glossopharyngeal nerve is fascinating. It originates from the medulla oblongata, which is the lower part of the brainstem. From there, it extends downwards and branches out into various regions of the head and neck. The nerve has multiple connections with other cranial nerves, allowing for coordinated and efficient functioning of the nervous system.
Anatomy of the Glossopharyngeal Nerve
The glossopharyngeal nerve is composed of several distinct components. The motor fibers of the nerve arise from the nucleus ambiguus, a cluster of nerve cell bodies located in the medulla oblongata. These motor fibers travel along the nerve and innervate the stylopharyngeus muscle, which is responsible for elevating the pharynx during swallowing.
On the other hand, the sensory fibers of the glossopharyngeal nerve originate from the superior and inferior ganglia. These ganglia contain sensory cell bodies that receive and transmit information from various structures. The sensory fibers carry taste sensations from the posterior one-third of the tongue, as well as general sensory information from the tonsils, pharynx, and middle ear.
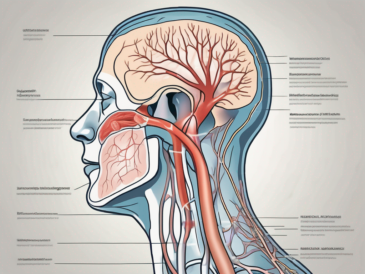
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve performs various important functions in the body. It facilitates swallowing by coordinating the movement of muscles in the throat. This coordination ensures that food and liquids are safely transported from the mouth to the esophagus, preventing choking or aspiration.
Another fascinating function of the glossopharyngeal nerve is its involvement in the sensation of taste. The nerve carries taste sensations from the posterior one-third of the tongue, allowing us to perceive flavors such as bitter and sour. This sensory information is crucial for our enjoyment of food and our ability to differentiate between different tastes.
In addition to its role in swallowing and taste sensation, the glossopharyngeal nerve also carries general sensory information from the throat, tonsils, and other structures in the head and neck region. This information is essential for maintaining our sense of touch, temperature, and pain perception in these areas.
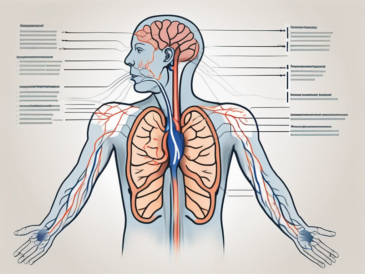
Furthermore, the glossopharyngeal nerve is involved in the regulation of blood pressure and heart rate. It contains specialized sensory receptors called baroreceptors, which detect changes in blood pressure. When these receptors sense a decrease in blood pressure, they send signals to the brainstem, which then activates the appropriate mechanisms to increase blood pressure and maintain cardiovascular homeostasis.
In conclusion, the glossopharyngeal nerve is a fascinating component of the cranial nerve system. Its intricate anatomy and diverse functions make it a vital part of our ability to swallow, taste, and perceive sensations in the head and neck region. Additionally, its involvement in cardiovascular regulation highlights the complex interplay between the nervous system and other physiological processes in the body.
Preparing for the Glossopharyngeal Nerve Test
Necessary Equipment for the Test
Prior to performing the glossopharyngeal nerve test, it is essential to gather the necessary equipment. The specific requirements may vary depending on the healthcare setting and the techniques employed. However, commonly used equipment may include a tongue depressor, flashlight, cotton swabs, and gloves to ensure proper infection control.
Let’s delve deeper into the equipment required for the glossopharyngeal nerve test. The tongue depressor is a vital tool used to examine the back of the patient’s throat. It helps to depress the tongue and provide a clear view of the area. A flashlight is used to illuminate the throat, enabling the healthcare provider to observe any abnormalities or irregularities. Cotton swabs are used to collect samples or apply substances to specific areas of the throat, if necessary. Gloves, on the other hand, are worn to maintain a sterile environment and prevent the spread of infection.
Patient Preparation Guidelines
Before proceeding with the test, it is crucial to obtain informed consent from the patient and explain the procedure in detail. Inform the patient about the purpose of the test, possible sensations they may experience, and any associated risks or complications. Ensure that the patient is comfortable and positioned appropriately, preferably in an upright position.
Now, let’s explore the patient preparation guidelines for the glossopharyngeal nerve test in more detail. Obtaining informed consent is a fundamental step in any medical procedure. It involves explaining the purpose of the test to the patient, ensuring they understand its significance in diagnosing or monitoring their condition. Additionally, informing the patient about the possible sensations they may experience during the test helps to alleviate any anxiety or discomfort they may feel.
Positioning the patient appropriately is crucial for a successful glossopharyngeal nerve test. Placing the patient in an upright position allows gravity to assist in the examination process. It also helps the healthcare provider to have a better view of the patient’s throat, making it easier to identify any abnormalities. Comfort is equally important, as it helps the patient relax and cooperate during the procedure.
By following these patient preparation guidelines and ensuring the availability of necessary equipment, healthcare providers can conduct a thorough and effective glossopharyngeal nerve test. This test plays a crucial role in diagnosing and managing various conditions related to the glossopharyngeal nerve, such as glossopharyngeal neuralgia or swallowing difficulties. The detailed preparation and attention to detail contribute to accurate results and improved patient outcomes.
Step-by-Step Procedure of the Glossopharyngeal Nerve Test
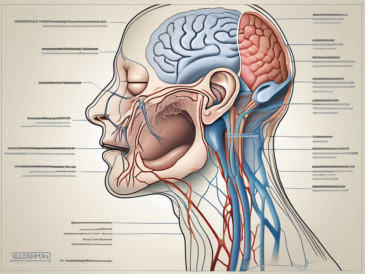
Initial Assessment
The initial assessment involves a comprehensive evaluation of the patient’s medical history, symptoms, and any previous relevant test results. This assessment can provide valuable insights into the potential underlying causes and guide the subsequent steps of the glossopharyngeal nerve test.
During the initial assessment, the healthcare provider will carefully review the patient’s medical records, paying close attention to any previous diagnoses or treatments related to the glossopharyngeal nerve. They will also inquire about the patient’s current symptoms, such as difficulty swallowing, throat pain, or changes in taste perception. Additionally, the provider may ask about any recent injuries or infections that could potentially affect the glossopharyngeal nerve.
Furthermore, the healthcare provider may conduct a physical examination to assess the patient’s overall health. This may involve checking vital signs, such as blood pressure and heart rate, and performing a general examination of the head and neck region. The provider will also inquire about any other medical conditions or medications that the patient is currently taking, as certain medications or underlying health conditions can affect the function of the glossopharyngeal nerve.
Performing the Test
To test the glossopharyngeal nerve, a combination of clinical examination techniques may be employed. This may include assessing the patient’s ability to swallow, performing a gag reflex test, evaluating taste perception, and examining the tonsils and back of the throat using a tongue depressor and flashlight. The specifics of the test may vary depending on the presenting symptoms and suspected underlying conditions.
During the test, the healthcare provider will first assess the patient’s ability to swallow. This can be done by asking the patient to take sips of water or eat small amounts of food while observing their swallowing mechanism. Any difficulties or abnormalities in swallowing may indicate a problem with the glossopharyngeal nerve.
Next, the provider may perform a gag reflex test. This involves gently stimulating the back of the patient’s throat with a tongue depressor to elicit a gag reflex response. A normal gag reflex indicates the proper functioning of the glossopharyngeal nerve.
In addition, the healthcare provider may evaluate the patient’s taste perception. This can be done by applying different tastes, such as sweet, sour, salty, and bitter, to the patient’s tongue and asking them to identify the taste. Impaired taste perception or an inability to distinguish between different tastes may suggest a problem with the glossopharyngeal nerve.
Furthermore, the provider will carefully examine the tonsils and back of the throat using a tongue depressor and flashlight. They will look for any abnormalities, such as redness, swelling, or masses, that could indicate an underlying condition affecting the glossopharyngeal nerve.
Throughout the test, the healthcare provider will communicate with the patient, explaining each step and addressing any concerns or questions they may have. The provider will also document their findings and observations to aid in the diagnosis and treatment planning process.
Interpreting the Results of the Glossopharyngeal Nerve Test
The glossopharyngeal nerve plays a crucial role in the functioning of the throat and tongue, and evaluating its performance through a comprehensive test is essential for diagnosing potential issues. Understanding the interpretation of the test results is vital in determining the next steps in patient care and treatment.
Normal Test Results
Normal test results bring relief and assurance to both the patient and the healthcare provider. When the glossopharyngeal nerve is functioning within the expected parameters, it indicates that the neural pathways responsible for swallowing, taste perception, and throat reflexes are intact and working properly.
During the test, the patient’s ability to swallow without any difficulty is a positive sign. It suggests that the glossopharyngeal nerve is effectively coordinating the muscles involved in the swallowing process. Additionally, the absence of pathological reflexes, such as an exaggerated gag reflex, further supports a normal interpretation of the test results.
Another aspect that contributes to a normal interpretation is the intact taste perception. The glossopharyngeal nerve carries taste sensations from the back of the tongue, and if the patient can accurately identify different tastes, it indicates that the nerve is transmitting signals correctly.
Furthermore, a visual examination of the tonsils and throat can provide valuable insights. If the tonsils and throat appear normal, without any signs of inflammation, redness, or other abnormalities, it suggests that the glossopharyngeal nerve is not being affected by any underlying issues.
All these findings, combined with the absence of any concerning symptoms related to the glossopharyngeal nerve, contribute to a normal interpretation of the test results. However, it is important to note that the interpretation should always be done by a qualified healthcare professional.
Abnormal Test Results
When the glossopharyngeal nerve test yields abnormal results, it raises concerns about potential issues with the nerve’s functionality. Abnormal findings may indicate underlying conditions that require further investigation and appropriate medical intervention.
One of the common signs of an abnormal test result is difficulty swallowing, also known as dysphagia. If the patient experiences challenges in swallowing food or liquids, it suggests that the glossopharyngeal nerve may not be effectively coordinating the muscles involved in the swallowing process.
Another abnormal finding is a weakened gag reflex. The gag reflex is a protective mechanism that prevents foreign objects from entering the airway. If the glossopharyngeal nerve is not functioning properly, the gag reflex may be diminished, potentially putting the patient at risk of aspiration.
Altered taste perception is another indicator of abnormal test results. If the patient reports a change in their ability to taste or identifies tastes inaccurately, it suggests that the glossopharyngeal nerve may not be adequately transmitting taste signals to the brain.
Additionally, abnormalities in the appearance of the tonsils or throat can be indicative of issues with the glossopharyngeal nerve. Infections, tumors, or other underlying medical conditions can affect the nerve’s functionality and manifest as visible changes in the throat area.
When abnormal test results are obtained, further investigations may be necessary to determine the underlying cause. These investigations may include additional diagnostic tests, imaging studies, or consultations with specialists to ensure an accurate diagnosis and appropriate treatment plan.
It is important to note that abnormal test results do not necessarily confirm a specific condition. They serve as an indication that further evaluation is required to identify the underlying cause and develop an effective management strategy.
In conclusion, interpreting the results of the glossopharyngeal nerve test is a critical step in assessing the nerve’s functionality and identifying potential issues. Normal test results provide reassurance, while abnormal results prompt further investigations to ensure appropriate patient care.
Potential Complications and Risks of the Test
Common Complications
The glossopharyngeal nerve test is generally safe; however, as with any medical procedure, there are potential risks involved. Common complications may include gagging or discomfort during the examination, minor bleeding due to the use of a tongue depressor, or an adverse reaction to any local anesthesia or disinfectants used. These complications are usually temporary and resolve without significant intervention.
During the glossopharyngeal nerve test, it is not uncommon for patients to experience some level of gagging or discomfort. This is because the test involves the insertion of a tongue depressor into the back of the throat, which can trigger the gag reflex. While this sensation can be unpleasant, it is generally short-lived and subsides once the tongue depressor is removed.
In rare cases, the use of a tongue depressor during the test may cause minor bleeding. This can occur if the tongue depressor accidentally scrapes against the delicate tissues of the throat. However, it is important to note that this bleeding is typically minimal and stops on its own. If excessive bleeding occurs, medical professionals are trained to address it promptly and appropriately.
Another potential complication of the glossopharyngeal nerve test is an adverse reaction to local anesthesia or disinfectants used during the procedure. Although these substances are generally well-tolerated, some individuals may have an allergic reaction or sensitivity to them. If this occurs, it is crucial to inform the healthcare provider immediately so that appropriate measures can be taken to manage the reaction and ensure the patient’s safety.
Managing Potential Risks
To minimize potential risks, it is essential to ensure proper hygiene and infection control measures throughout the test. Adhering to aseptic techniques and using appropriate sterilization methods for equipment can significantly reduce the risk of complications. Healthcare professionals involved in the procedure should follow strict hand hygiene protocols and wear appropriate personal protective equipment to prevent the spread of infection.
In addition to maintaining a sterile environment, close monitoring and careful observation of the patient’s response during the procedure can aid in promptly addressing any complications or discomfort. Healthcare providers should be attentive to the patient’s verbal and non-verbal cues, such as signs of distress or increased gagging, and respond accordingly. Promptly addressing any concerns or complications can help ensure the patient’s comfort and safety throughout the test.
Furthermore, healthcare professionals should provide clear instructions and explanations to the patient before the test, ensuring that they understand what to expect and how to communicate any discomfort or complications that may arise. Open communication between the patient and the healthcare team can help build trust and facilitate a smoother testing experience.
Post-Test Care and Follow-up
Immediate Post-Test Care
After completing the glossopharyngeal nerve test, it is important to provide clear instructions to the patient regarding any necessary post-test care. This may include advice to rest and avoid strenuous activities for a short period, avoiding hot or spicy foods or drinks, and recommendations for pain management, if needed. Any temporary discomfort or side effects should be explained to the patient and reassurances provided.
Long-Term Follow-up and Management
Depending on the test results and suspected underlying conditions, the healthcare provider may recommend further investigations or consultations with relevant specialists. A comprehensive management plan can then be tailored to address the specific concerns and optimize the patient’s overall well-being. Close follow-up appointments can help monitor progress, assess the effectiveness of any interventions, and make necessary adjustments to the treatment plan, if required.
In conclusion, testing the glossopharyngeal nerve can provide valuable diagnostic information and aid in determining the underlying cause of certain symptoms. Proper understanding of the anatomy, careful preparation, step-by-step execution of the test, accurate interpretation of results, and appropriate post-test care and follow-up are crucial in obtaining reliable information. However, it is important to remember that this article has provided a general overview and does not substitute medical advice. If you have any concerns regarding your glossopharyngeal nerve function or suspect any related issues, it is strongly advised to seek the guidance of a qualified healthcare professional.