The glossopharyngeal nerve plays a crucial role in various functions of the head and neck region. Any damage to this nerve can result in several clinical signs and symptoms that may significantly impact an individual’s quality of life. Understanding the anatomy, functions, causes, diagnostic procedures, treatment options, and prognosis associated with glossopharyngeal nerve damage is paramount to effectively manage this condition.
Understanding the Glossopharyngeal Nerve
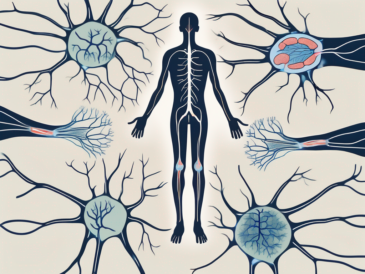
The glossopharyngeal nerve, also known as cranial nerve IX, is one of the twelve paired cranial nerves originating from the brainstem. It emerges from the medulla oblongata and consists of both sensory and motor fibers. This nerve innervates various structures, including the throat, tongue, middle ear, and certain glands. Its sensory functions are essential for taste perception, swallowing, and monitoring blood pressure, while its motor functions control the muscles involved in swallowing and speech articulation.
The glossopharyngeal nerve plays a crucial role in the complex network of nerves that govern the intricate movements and sensations of the head and neck region. Understanding its anatomy and functions is essential for comprehending the intricate workings of the human nervous system.
Anatomy of the Glossopharyngeal Nerve
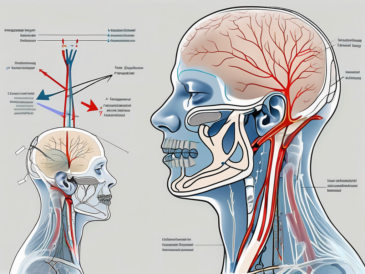
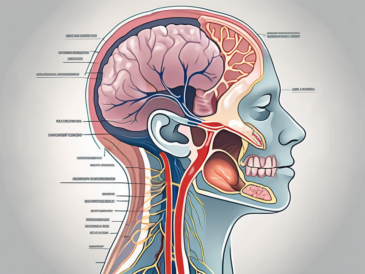
The glossopharyngeal nerve originates from the posterior aspect of the medulla oblongata, specifically from the nucleus ambiguus and the inferior salivatory nucleus. It leaves the skull through the jugular foramen along with the vagus and spinal accessory nerves. The jugular foramen is a small opening located at the base of the skull, allowing these vital nerves to exit the cranial cavity and reach their respective destinations.
Once outside the skull, the glossopharyngeal nerve branches into multiple fibers, each with its own unique pathway and function. These branches innervate different regions of the head and neck, ensuring the proper functioning of various structures and systems.
One branch of the glossopharyngeal nerve extends towards the tongue, providing sensory information and taste perception from the posterior third of the tongue. This allows us to savor the flavors of different foods and beverages. Another branch reaches the throat and middle ear, providing general sensation and contributing to our ability to swallow and perceive sound.
Furthermore, the glossopharyngeal nerve also carries taste sensations from the circumvallate papillae, which are large taste buds located towards the back of the tongue. These taste buds play a crucial role in our ability to detect and differentiate between different tastes, such as sweet, sour, bitter, and salty.
Functions of the Glossopharyngeal Nerve
The glossopharyngeal nerve serves multiple crucial functions, making it an indispensable component of our nervous system. Its sensory fibers carry taste sensations from the posterior third of the tongue, allowing us to enjoy the diverse flavors of the foods we consume. Additionally, the glossopharyngeal nerve plays a vital role in monitoring blood pressure through the carotid sinus baroreceptors.
The carotid sinus baroreceptors are specialized sensory receptors located in the carotid arteries, which are major blood vessels in the neck. These receptors constantly monitor the blood pressure and relay this information to the brain via the glossopharyngeal nerve. This feedback loop helps regulate blood pressure and maintain homeostasis within the body.
Moreover, the glossopharyngeal nerve provides general sensation to the throat and middle ear, allowing us to perceive and respond to various stimuli in these regions. This sensory input is crucial for maintaining proper function and protecting these delicate structures from potential harm.
On the motor side, the glossopharyngeal nerve controls the muscles involved in swallowing and speech articulation. These muscles work in harmony to facilitate the complex process of swallowing, allowing us to consume food and drink without difficulty. Additionally, the glossopharyngeal nerve plays a role in speech articulation, allowing us to form and pronounce words clearly and effectively.
In summary, the glossopharyngeal nerve is a remarkable cranial nerve that plays a vital role in our daily lives. From enabling us to taste and enjoy food to regulating blood pressure and facilitating essential functions like swallowing and speech, this nerve is an integral part of our intricate nervous system.
Causes of Glossopharyngeal Nerve Damage
Glossopharyngeal nerve damage can occur due to various reasons, including trauma, injury, medical conditions, and diseases.
The glossopharyngeal nerve, also known as the ninth cranial nerve, is responsible for providing sensation to the back of the throat and tongue, as well as controlling certain muscles involved in swallowing and speech. When this nerve is damaged, it can lead to a range of symptoms and complications.
Trauma and Injury
Direct trauma to the head, neck, or skull can lead to glossopharyngeal nerve damage. This can occur due to accidents, falls, or sports-related injuries. For example, a severe blow to the head during a car accident can cause the nerve to become compressed or stretched, leading to damage.
In addition to external trauma, surgical procedures in the vicinity of the glossopharyngeal nerve can also result in nerve injury. Surgeons must exercise extreme caution and precision when operating in this delicate area to minimize the risk of nerve damage.
Rehabilitation and physical therapy are often necessary to help individuals recover from glossopharyngeal nerve damage caused by trauma or injury. These treatments focus on improving muscle strength and coordination, as well as restoring normal swallowing and speech function.
Medical Conditions and Diseases
Certain medical conditions and diseases can also cause damage to the glossopharyngeal nerve. One example is the presence of tumors in the head and neck region. These tumors can exert pressure on the nerve, leading to compression and subsequent damage.
Infections such as glossopharyngeal neuralgia, a condition characterized by severe pain in the throat and tongue, can also affect the glossopharyngeal nerve. The inflammation and irritation caused by the infection can disrupt the normal functioning of the nerve, resulting in damage.
Systemic conditions like diabetes or multiple sclerosis can also contribute to glossopharyngeal nerve damage. In diabetes, high blood sugar levels can lead to nerve damage throughout the body, including the glossopharyngeal nerve. Similarly, multiple sclerosis, an autoimmune disease that affects the central nervous system, can cause inflammation and damage to the nerves, including the glossopharyngeal nerve.
Early diagnosis and appropriate management of these underlying conditions are crucial to prevent further damage to the glossopharyngeal nerve. Treatment may involve medications to control pain and inflammation, as well as addressing the underlying cause of the nerve damage.
In conclusion, glossopharyngeal nerve damage can occur due to various reasons, including trauma, injury, medical conditions, and diseases. It is important to be aware of the potential causes and take necessary precautions to minimize the risk of damage to this vital nerve. Prompt diagnosis and appropriate management of any underlying conditions are essential for preventing further complications and promoting recovery.
Clinical Signs of Glossopharyngeal Nerve Damage
The glossopharyngeal nerve plays a crucial role in various functions related to the tongue, throat, and middle ear. When this nerve is damaged, it can lead to a range of clinical signs and symptoms that vary depending on the extent and location of the injury.
Sensory Symptoms
One of the primary sensory symptoms associated with glossopharyngeal nerve damage is altered taste perception. Specifically, individuals may experience changes in taste sensation in the posterior third of the tongue. This can result in a diminished or altered sense of taste for food and liquids. Imagine biting into your favorite dish, only to find that the flavors are muted or distorted.
In addition to taste disturbances, individuals with glossopharyngeal nerve damage may also report pain or discomfort in the throat or middle ear region. This can manifest as a persistent sore throat or a nagging earache. These sensory symptoms can be distressing and may significantly impact an individual’s overall quality of life.
It is important to note that these sensory symptoms may overlap with other conditions, making an accurate diagnosis challenging. Therefore, a thorough evaluation by a healthcare professional is necessary to determine the underlying cause of these symptoms and develop an appropriate management plan.
Motor Symptoms
Glossopharyngeal nerve damage can also lead to motor symptoms that primarily affect swallowing and speech articulation. Impairments in swallowing can make it difficult for individuals to consume solid or liquid food, increasing the risk of choking episodes or aspiration. Imagine the frustration and fear of not being able to enjoy a meal without the constant worry of choking.
Speech articulation may also be affected in individuals with glossopharyngeal nerve damage. This can result in slurred speech or difficulties in pronouncing certain sounds or words. Imagine struggling to communicate clearly, feeling self-conscious about your speech, and having others struggle to understand you.
If you are experiencing any of these motor symptoms, it is crucial to seek medical attention promptly. A healthcare professional can evaluate your condition, conduct necessary tests, and recommend appropriate interventions to improve your swallowing and speech abilities. Early intervention can make a significant difference in your ability to eat, communicate, and maintain a good quality of life.
In conclusion, glossopharyngeal nerve damage can have a profound impact on sensory and motor functions related to the tongue, throat, and middle ear. Altered taste perception, throat or ear pain, difficulties in swallowing, and speech articulation impairments are some of the clinical signs and symptoms associated with this condition. Seeking timely medical attention is essential to accurately diagnose the underlying cause and develop an appropriate treatment plan tailored to your specific needs.
Diagnostic Procedures for Glossopharyngeal Nerve Damage
In diagnosing glossopharyngeal nerve damage, a comprehensive assessment is imperative to identify the underlying cause and extent of the nerve injury.
Glossopharyngeal nerve damage can result from various factors, including trauma, infections, tumors, or systemic conditions. To accurately diagnose the condition, healthcare professionals employ a range of diagnostic procedures that provide valuable insights into the nature and severity of the nerve damage.
Physical Examination
A thorough physical examination by a healthcare professional is the first step in diagnosing glossopharyngeal nerve damage. During this assessment, the healthcare professional will evaluate various aspects related to the functioning of the glossopharyngeal nerve.
One crucial aspect of the physical examination is the assessment of sensory perception. The healthcare professional will test the patient’s ability to perceive sensations in the throat and surrounding areas. This evaluation helps determine if there is any loss or alteration in sensory function, which can indicate glossopharyngeal nerve damage.
Speech and language evaluation is another important component of the physical examination. The healthcare professional will assess the patient’s ability to articulate words and phrases clearly. Any difficulties or abnormalities in speech patterns may suggest glossopharyngeal nerve involvement.
Furthermore, the examination will include an evaluation of swallowing abilities. The healthcare professional will observe the patient’s ability to swallow food and liquids without difficulty. They will pay special attention to the gag reflex, tongue movement, and signs of muscle weakness in the throat and face, as these can indicate glossopharyngeal nerve damage.
Additionally, specific tests targeting the glossopharyngeal nerve, such as the glossopharyngeal provocation test, may be performed to aid in diagnosis. This test involves stimulating the glossopharyngeal nerve and observing the patient’s response, helping to identify any abnormalities or deficits.
Imaging and Laboratory Tests
In addition to the physical examination, healthcare professionals may utilize imaging and laboratory tests to further evaluate glossopharyngeal nerve damage.
Imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, can provide detailed images of the head, neck, and throat regions. These images help identify any tumors, lesions, or structural abnormalities that may be causing glossopharyngeal nerve damage. By visualizing the affected area, healthcare professionals can better understand the extent and nature of the nerve injury.
Furthermore, blood tests or cerebrospinal fluid analysis may be conducted to evaluate for systemic conditions or infections that could be contributing to glossopharyngeal nerve damage. These tests help identify any underlying medical conditions that may require specific treatment or management.
It is essential to collaborate with a healthcare professional to determine the most appropriate diagnostic tests for your specific case. Their expertise will guide the diagnostic process and ensure accurate identification of the underlying cause of your glossopharyngeal nerve damage.
Remember, early diagnosis and intervention are crucial in managing glossopharyngeal nerve damage effectively. Seeking medical attention and undergoing the necessary diagnostic procedures will help healthcare professionals develop an appropriate treatment plan tailored to your needs.
Treatment Options for Glossopharyngeal Nerve Damage
Management of glossopharyngeal nerve damage focuses on addressing the underlying cause and alleviating the associated symptoms. Glossopharyngeal nerve damage can result from various factors, including trauma, infection, or compression of the nerve.
When it comes to treating glossopharyngeal nerve damage, there are several options available, ranging from medication and therapy to surgical interventions. The choice of treatment depends on the specific cause and severity of the nerve damage.
Medication and Therapy
In cases where glossopharyngeal neuralgia is the cause of nerve damage, medications such as anticonvulsants or tricyclic antidepressants may be prescribed to manage pain and reduce nerve irritation. These medications work by altering the way nerve signals are transmitted, providing relief from pain and discomfort.
Physical therapy or swallowing therapy can also be beneficial in improving swallowing abilities and increasing muscle strength in the throat. These therapies involve exercises and techniques designed to strengthen the muscles involved in swallowing and improve coordination. They can be particularly helpful in cases where glossopharyngeal nerve damage has resulted in difficulty swallowing or a weak gag reflex.
It is essential to note that medication and therapy recommendations should only be followed under the guidance of a healthcare professional. They can assess your specific case and tailor a treatment plan to your individual needs. A healthcare professional will consider factors such as the severity of the nerve damage, the presence of any underlying conditions, and your overall health before recommending a specific course of treatment.
Surgical Interventions
In some instances, surgical interventions may be necessary to address the underlying cause of glossopharyngeal nerve damage. This may include the removal of tumors or lesions compressing or invading the nerve. Surgery aims to relieve pressure on the nerve and restore its normal function.
Before considering surgery, a thorough evaluation and discussion with a qualified surgeon are essential. The surgeon will assess the extent of the nerve damage, identify the underlying cause, and determine the most appropriate surgical approach. They will also discuss the potential risks and benefits of the procedure, allowing you to make an informed decision about your treatment.
Surgical interventions for glossopharyngeal nerve damage are typically performed by neurosurgeons who specialize in treating conditions affecting the nervous system. These highly skilled professionals have the expertise and experience to perform complex procedures while minimizing the risk of complications.
In conclusion, the treatment options for glossopharyngeal nerve damage are varied and depend on the underlying cause and severity of the condition. Medications and therapy can help manage pain and improve swallowing abilities, while surgical interventions may be necessary to address the root cause of the nerve damage. It is crucial to consult with a healthcare professional to determine the most appropriate treatment plan for your specific case.
Prognosis and Recovery from Glossopharyngeal Nerve Damage
The prognosis and recovery from glossopharyngeal nerve damage can vary greatly depending on the cause, extent of nerve damage, and individual factors.
Factors Influencing Recovery
The underlying cause of the nerve damage plays a significant role in determining the potential for recovery. In cases where the damage is due to trauma or injury, a better prognosis may be expected compared to damage caused by progressive medical conditions or systemic diseases. Additionally, the timeliness of diagnosis, appropriate management, and the individual’s overall health and adherence to treatment can also influence recovery.
Coping and Rehabilitation Strategies
Coping with glossopharyngeal nerve damage requires a holistic approach that focuses on improving functionality and quality of life. Rehabilitation strategies, including speech therapy and swallowing exercises, can help individuals regain or adapt to their swallowing and speech abilities. Additionally, support from healthcare professionals, family, and friends can play a crucial role in providing emotional support and understanding throughout the recovery process.
It is important to remember that each case of glossopharyngeal nerve damage is unique, and outcomes can vary. Consulting with a healthcare professional who specializes in the management of nerve injuries can provide valuable guidance and support tailored to your specific needs.
In conclusion, damage to the glossopharyngeal nerve can lead to various clinical signs and symptoms that significantly impact an individual’s daily life. Understanding the anatomy, functions, causes, diagnostic procedures, treatment options, and prognosis associated with this condition is vital. By seeking prompt medical attention and collaborating with healthcare professionals, individuals can receive appropriate care and support, facilitating their recovery and enhancing their overall well-being.